To be sure, Prior Authorization (PA) is a pain point for payers, physicians, and patients alike. Obtaining advance permission from a payer before a covered drug is dispensed is time consuming and frustrating. Until recently, nearly all PAs required submissions of information via phone, fax, and portals. But that is changing with the availability of electronic prior authorization (ePA) for drugs covered under the patient’s pharmacy benefit, the capability for which has now reached an inflection point. This will have major implications for biopharma companies because an increasing number of drugs require PA, medications don’t get dispensed until approved, and healthcare is rapidly becoming automated. This article explains why and how biopharma companies should be preparing now for the anticipated surge of ePA adoption on the near-term horizon.
ePA is among the transactions that are revolutionizing prescribing at the point of care. While its uptake has not advanced as quickly as many would like, several drivers are accelerating ePA adoption, including:
Infrastructure
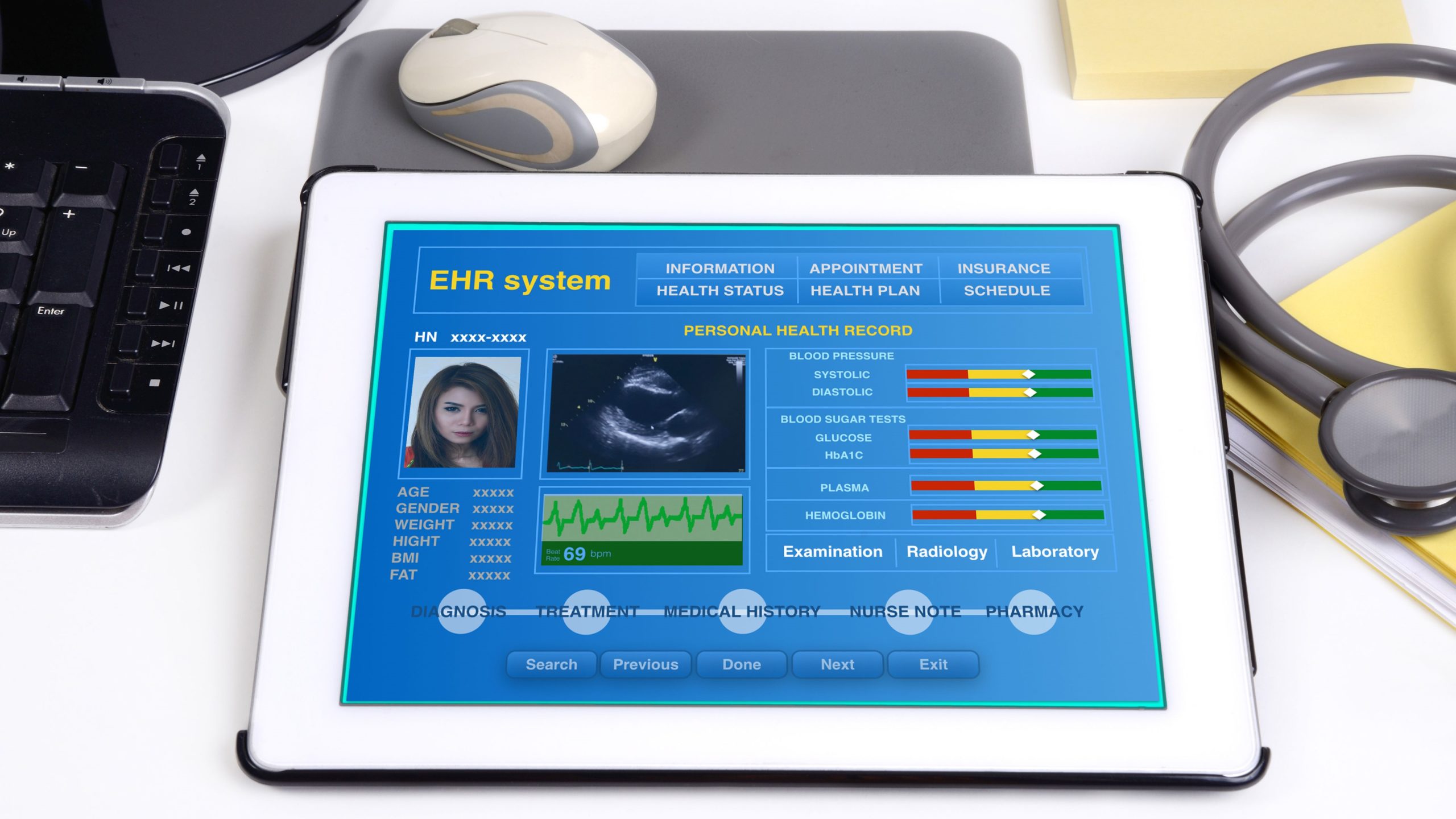
- The National Council for Prescription Drug Programs (NCPDP)’s SCRIPT version 20170701 has been rolled out, making ePA transactions more robust and offering the ability for real-time ePAs.
- Many electronic health records systems (EHRs), intermediaries, and payers have integrated ePA into their systems.
The shift to value-based care
- The volume and complexity of PAs is increasing pressure to reduce administrative burden and costs with automation as value-based care arrangements expand.
- Manual PA costs providers about $11/each to process vs. $1.88 for ePA transactions, potentially saving healthcare $454 million annually.
Federal and state regulations
- Medicare Part D will require ePA transactions that are supported using the NCPDP standard beginning on Jan 1, 2021. Thirty states allow ePA, and others have mandates in consideration.
- Insurers tend to follow Medicare’s lead.
Stakeholder involvement
- Several leading payers, health IT vendors, and standards groups are driving to advance ePA.
- America’s Health Insurance Plans (AHIP), a major insurance industry group, and several member insurers (covering 60 million lives) recently launched an ePA pilot program.
In addition to these drivers, the shift to automating PA is happening because of the well-recognized benefits. For example, ePA can dramatically cut the burden of processing PA requests. Physicians and their staff spend an average of two days per week in processing PAs. This translates into nearly $70,000 annually per physician office. Nearly 40% of PA requests (roughly 75 million) annually are abandoned due to complexities and delays associated with manual PA. ePA can help both providers and payers address medication non-adherence. This is a patient safety issue and costs the healthcare system some $100-$289 billion annually in preventable deaths; unnecessary doctor and hospital visits; and needless hospital and nursing home admissions. ePA is also a tool to help prevent the diversion and unnecessary dispensing of opioids.
Biopharma companies can take these five steps to ensure ePA is a successful part of planning and operations:
- Learn the latest updates on ePA. Ensure you are thoroughly grounded in ePA. What is it? How does it work? How will it be used for their brands?
- Include ePA in payer marketing strategies. Understand how ePA impacts brands. Consider how PA requirements and ePA processes will impact prescriber and patient experiences, and what regulations are in play. Then fold the findings into planning and strategy development.
- Understand the implications of ePA in EHRs. It is critically important to know how brands are presented in various EHRs and how documentation requirements for different payers will be managed.
- Include ePA in sales force training. Understand how the required level of effort may impact doctors and practices, and train the sales force to be a resource for education. Physicians and staff will need to be educated on how ePA could work in their EHR and how it can positively impact their workflow.
- Get involved. Two standards development organizations—NCPDP and Health Level Seven (HL7)—are having a profound impact on ePA, and are in dire need of the biopharma perspective. These organizations represent an opportunity to advocate for more automation and help ensure industry objectives are understood and met. This is especially important as the industry moves to expand the use of ePA for drugs and devices covered under the patient’s medical benefit (which account for about half of all PA from a spend-standpoint). Also consider either monitoring or getting involved in the numerous stakeholder collaborations aimed at streamlining PA, accelerating adoption, and reducing provider burden.
Like ePrescribing before it, biopharma companies can successfully leverage ePA through planning, education, and stakeholder collaboration. There is no time like the present.