Marketers often target specialists to increase awareness about specialty medication, but this case study examines why it is important to also engage with primary care providers and what makes the EHR an effective way to reach both.
THE CHALLENGE
Medications for chronic illnesses—such as depression—may initially be prescribed by a specialist; but ongoing care for chronic conditions frequently occurs in the primary care setting. Traditionally, specialty medication marketing targets specialists, bypassing those general practitioners who would benefit from the medication information.
Although Depression Clearly Qualifies as a Mental Health Disorder, Primary Care Physicians (PCPs) Have Become the Most Likely Providers to Handle Its Diagnosis and Treatment, Not Specialists1, 2
Major depressive disorder (MDD) is a serious health condition. The World Health Organization identifies depression as the leading cause of disability worldwide, affecting 4.4% of the global population. It’s also a major risk factor for completed suicide, suicide attempts, and self-harm.1 According to the National Alliance on Mental Illness (NAMI), suicide is currently the 12th leading cause of death in the U.S.3
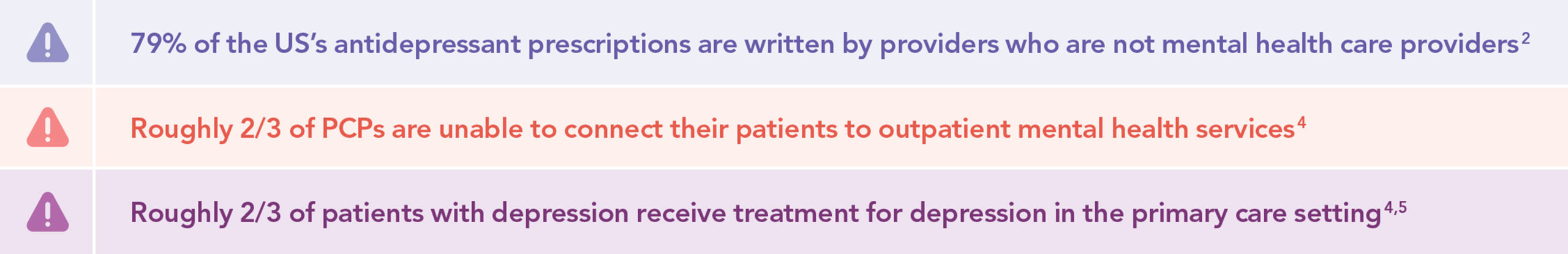
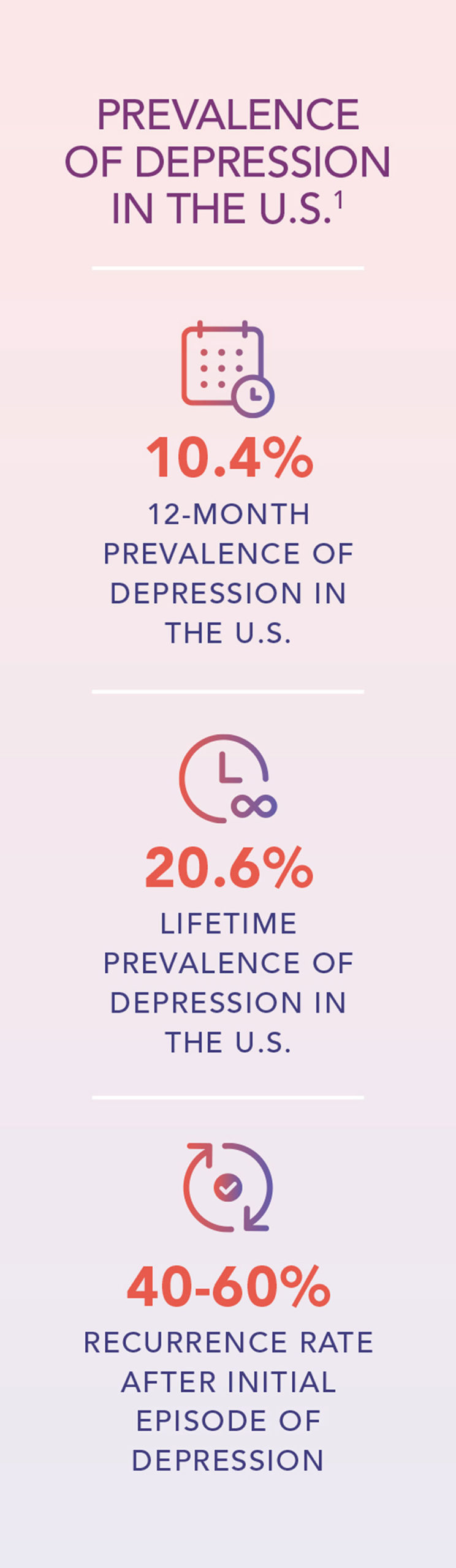 A position paper from the American Academy of Family Physicians (AAFP) states that about two out of every three patients with depression receive treatment for it in the primary care setting.4, 5 PCPs are usually a patient’s first contact with the healthcare system, which can give them the opportunity to detect depression at an early stage.6, 7 PCPs can then elect whether to treat the patient themselves or refer the patient to a specialist.
A position paper from the American Academy of Family Physicians (AAFP) states that about two out of every three patients with depression receive treatment for it in the primary care setting.4, 5 PCPs are usually a patient’s first contact with the healthcare system, which can give them the opportunity to detect depression at an early stage.6, 7 PCPs can then elect whether to treat the patient themselves or refer the patient to a specialist.
However, the stigma associated with depression makes many patients reluctant to seek out a specialist.1 As a result, roughly two out of every three PCPs are unable to connect their patients with depressive symptoms to outpatient mental health services;4 of patients who are referred to specialists, about 50% will fail to make their first appointment.8
Another challenge is that mental healthcare specialists are frequently in short supply, especially in rural areas. More than 25 million rural Americans live in an official Mental Health Professional Shortage Area, where there are too few mental health providers to care for those needing their services.1, 3 The Health Resources and Services Administration (HRSA) projects that shortages will continue to worsen, predicting that by 2030 there will be a shortage of 12,530 adult psychiatrists despite the growing demand.8
These factors combine to bring many patients to continue depression treatment in primary care. Even when patients are referred to psychiatrists, their PCPs often take over the role of prescribing medication refills once the patient’s condition is stable.5 As a result, 79% of prescriptions for antidepressant medications are written by providers who are not mental health care specialists.2
This decision is further supported by recent research showing that similar outcomes can be achieved when antidepressant medications are prescribed in the primary care setting as when they are prescribed by a specialist.8, 9 The Collaborative Mental Health Care Task Force of the World Federation of Societies of Biological Psychiatry published a position paper in which they advocated for incorporating primary care providers into the delivery of mental health services as the only way to meet the population’s mental health needs.7
 Increasing Market Awareness was a Challenge, Requiring Connections with PCPs as well as Specialists
Increasing Market Awareness was a Challenge, Requiring Connections with PCPs as well as Specialists
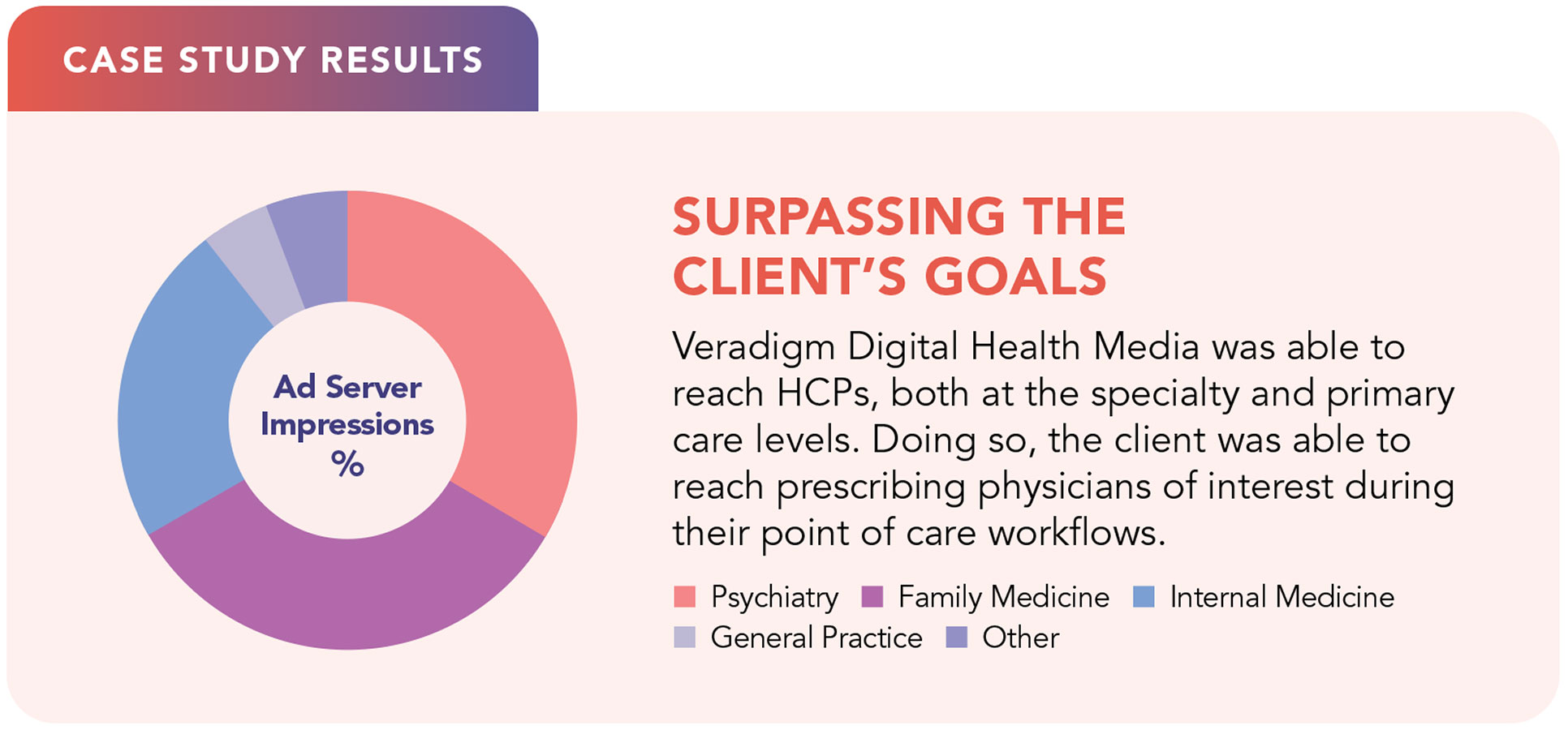
The medication referenced in this case study is a prescription medication used for the treatment of MDD in adults. The marketing team supporting this medication wanted to increase market awareness of the medication, and they wanted to do so with healthcare providers who were actively involved in the diagnosis and treatment of adult patients with MDD. Their objective was to reach both psychiatrists and PCPs who did not specialize in mental healthcare but dealt with patients who might have MDD.
However, research shows that physicians are typically extremely difficult to reach using traditional internet marketing. The 2022 Medscape Physician Lifestyle and Happiness Report notes that many physicians today spend less than 10 non-working hours online weekly, in contrast to the average U.S. internet user, who spends nearly 7 hours online every day.10
THE SOLUTION
Veradigm Digital Health Media is unique because it enables marketing teams to reach specific types of physicians and to reach them during their normal daily workflow.
Although physicians spend notably less time online than average, they spend a great deal of time interacting with their electronic health record (EHRs)—an average of 4.5 hours a day, according to one report.11 Another study found that physicians spend an average of 16 minutes using their EHRs per patient encounter.12
Veradigm Digital Health Media was able to focus the approved messaging to physicians of interest based on their client lists, prescribing history, or the use of specific ICD-10 codes. This allowed the marketing team to deliver messaging to the physicians of interest—those who would benefit from knowledge of a medication indicated for use in the treatment of adult depression.
Veradigm Digital Health Media Could Deliver the Client’s Message to the Right Physician Types:
- Specialists
- PCPs diagnosing or treating patients with MDD
Veradigm Digital Health Media Could Deliver the Client’s Message to Target Physicians at the Right Time and Place:
- During providers’ normal workflow
- Via EHRs, where providers spend an average of 4.5 hours per day
Veradigm’s ability to reach providers through their normal EHR use means providers are accessible far more often than they would be through other promotional options. In contrast, when advertisers attempted to target a group of physicians with banner ads, they found that 80% of physicians didn’t even see the banners, which were blocked by ad blocking software.13
 Try Veradigm Digital Health Media to Deliver Your Messaging to Physicians of Interest
Try Veradigm Digital Health Media to Deliver Your Messaging to Physicians of Interest
Veradigm enables biopharmaceutical marketers to deliver their awareness messages directly to physicians of interest, and to do so during their point of care workflow. Although today’s healthcare providers spend much less time online than the average American, they spend hours interacting with their EHRs. That is when approved medication messaging is available to them.
Contact us to learn more about Veradigm Digital Health Media and how we can help you reach the specific physicians in your target market.
CONTACT US veradigm.com/contact OR VISIT US AT veradigm.com
References:
1. Feldman E, MD. “Diagnosis, Treatment, and Management of Depression: The Role of the Primary Care Provider.” Relias Media. Updated January 1, 2021. Accessed September 1, 2022, https://www.reliasmedia.com/articles/147339-diagnosis-treatment-and-management-of-depression-the-role-of-the-primary-care-provider.
2. Park LT, MD, Zarate CA, MD. “Depression in the Primary Care Setting.” N Engl J Med. February 7, 2019;380(6):559-568. doi:10.1056/NEJMcp1712493.
3. “Mental Health by the Numbers.” National Alliance on Mental Illness (NAMI). Updated June 2022. Accessed September 1, 2022, https://www.nami.org/mhstats.
4. “Mental Health Care Services by Family Physicians (Position Paper).” American Academy of Family Physicians (AAFP). Accessed September 1, 2022, https://www.aafp.org/about/policies/all/mental-health-services.html.
5. “Your Primary Care Provider Can Help Treat Your Mental Health, Too.” University Hospitals. Updated March 21, 2021. Accessed September 1, 2022, https://www.uhhospitals.org/Healthy-at-UH/articles/2021/03/your-primary-care-provider-can-help-treat-your-mental-health-too.
6. Trautmann S, Beesdo-Baum K, Knappe S, et al. “The Treatment of Depression in Primary Care—A Cross-sectional Epidemiological Study.” Deutsches Ärzteblatt International. October 2017;114(43):721-728. doi:10.3238/arztebl.2017.0721.
7. Kates N, Arroll B, Currie E, et al. “Improving Collaboration Between Primary Care and Mental Health Services.” The World Journal of Biological Psychiatry: the Official Journal of the World Federation of Societies of Biological Psychiatry. June 20, 2018;20(10):748-765. doi: https://doi.org/10.1080/15622975.2018.1471218.
8. Kieu A, MD. “Now More Than Ever, Mental Health Care Needs Family Medicine. Opinion.” Fam Pract Manag. 2021;28(3):11A-11C.
9. Bogucki OE, Williams MD, Solberg LI, Rossom RC, Sawchuk CN. “The Role of the Patient-Centered Medical Home in Treating Depression.” Current Psychiatry Reports. July 14, 2020;22:47. doi: https://doi.org/10.1007/s11920-020-01167-y.
10. Baggett SM, Martin KL. “Medscape Physician Lifestyle & Happiness Report 2022.” Medscape. Updated January 14, 2022. Accessed March 9, 2022, https://www.medscape.com/slideshow/2022-lifestyle-happiness-6014665.
11. Overhage JM, McCallie D. “Physician Time Spent Using the Electronic Health Record During Outpatient Encounters.” Annals of Internal Medicine®. February 4, 2020;172(3):169-174. doi: https://doi.org/10.7326/M18-3684.
12. Gogineni T, Kahn J, Maya S. “How Much Time Do Physicians Spend in the EHR?” MedPage Today. Updated April 10, 2022. Accessed June 10, 2022, https://www.kevinmd.com/2022/04/how-much-time-do-physicians-spend-in-the-ehr.html.
13. Benko B. “Banner Ads Don’t Work on U.S. Physicians.” Forbes. Updated May 13, 2019. Accessed June 11, 2022, https://www.forbes.com/sites/forbestechcouncil/2019/05/13/banner-ads-dont-work-on-u-s-physicians/?sh=52c2f1343dbb.
* Veradigm Digital Health Media services operate in a manner that is in compliance with HIPAA and other applicable laws. In addition, the EHR displays advertisements in an iframe window adjacent to the EHR workflow that is separate and distinguishable from the clinical and practice management workflow within the EHR. No biopharma or device advertisements appear during the prescribing workflow.









