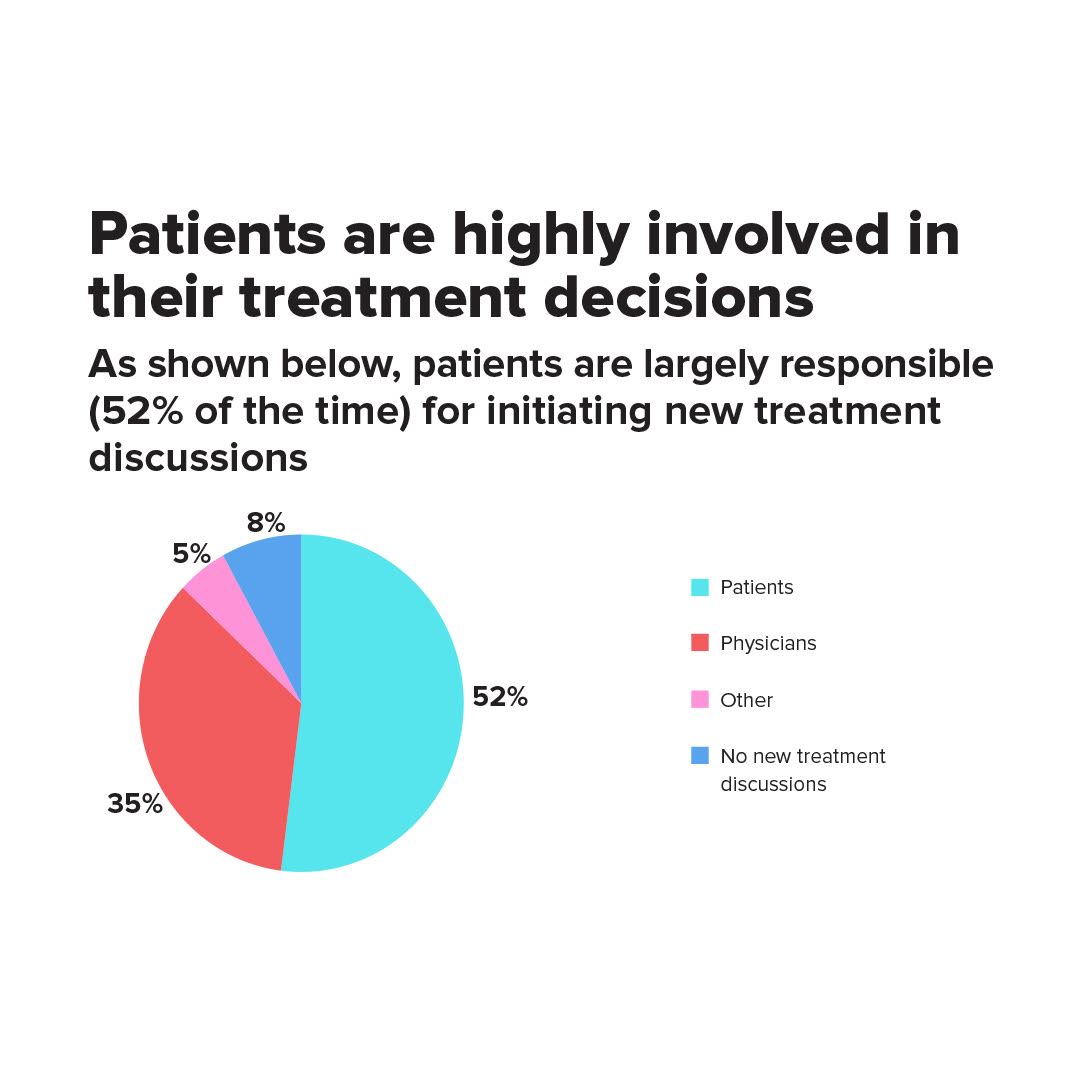
If patient centricity still isn’t an imperative to pharma, it probably should be! A recent survey revealed more than half of patients initiate new treatment discussions. According to the inaugural Inspire Survey, 52% of the 13,633 patients surveyed (from within Inspire’s health support communities for patients and caregivers) initiate new treatment discussions with their physicians. In fact, 45% of patients ask about another treatment at least once every other visit, while 89% ask about another treatment about once per year.
“A lot of patients are now making decisions that affect how their dollars are spent and that has increased the level of interest we get from pharma to learn more about patient decision making,” explains Brian Loew, CEO of Inspire. “Whereas 20 years ago it was much easier to imagine a situation in which a patient goes to the doctor and then uses whatever the doctor recommends, patients now want to express opinions and have conversations about treatment options. Because of that, pharma companies care a lot more about how patients make those decisions, what influences them, what they’re thinking and what’s important to them—in the past they didn’t have to think about that.”
An increased shared decision-making trend is also reflected in the survey. Nearly 70% of patients said they make collaborative treatment decisions with their doctor, while 20% said the decision is made “mostly” or “entirely” by them, and only 11% said the decision is “mostly” or “entirely” left up to the physician. Unsurprisingly, the younger patients are driving this trend. Respondents in the under 30-year-old age group asked about other treatment options most frequently; those between 31-40 and 41-50 asked at relatively the same rate, followed by respondents 51-64 who asked less frequently then the aforementioned groups. Finally, respondents 65+ asked least frequently about new treatment options, according to Dave Taylor, Director of Research at Inspire.
Patients Relationships with Pharma
What may also come as little shock to anyone in this industry: Patients report having a very limited relationship with pharma companies. Only 12% of patients felt that they had any kind of “relationship” with the companies that made their medications, although that number was slightly more prevalent among Autoimmune patients. Next came Respiratory, Metabolic and Neurologic patients who all rated their relationship with pharma as fairly similarly while Oncology respondents least commonly reported a relationship with pharma. However, according to Taylor, when asked about the perceived quality of this relationship (“limited” vs. “good”), the findings were consistent across all five groups and were in line with the overall average.
Additionally, few patients are even aware who makes their drugs. A reported 35% of patients didn’t know any of the pharmaceutical companies responsible for making the products they use; 37% knew some of the companies; 17% knew most of the companies; and only 10% knew all of the companies. While rare disease patients weren’t included in the survey, Loew believes the numbers would be higher for them in terms of knowing who makes their medications and also having some kind of a relationship with that pharma company.
“In our experience rare disease patients are well educated or become well educated after diagnosis about which treatments are available to them,” adds Loew. “And there is a lot of conversation in Inspire about upcoming treatments—a lot of anticipation—patients are researching the medical literature, they are looking at clinical trials before they even reach the market, they are talking about all of the potential treatments.”
The Tools and Resources Patients Want
These empowered patients use a number of resources to find information about their disease or treatment options including condition-specific websites (78%); online search engines (76%); medical/scientific articles (51%); online support communities (49%); and books or magazines (42%). While the survey did not distinguish what defines a “condition-specific websites,” Taylor says that based on prior client-sponsored research by Inspire, patients use both pharma-sponsored as well as “independent” websites for information, but the independent websites/sources are more desirable as pharma-sponsored content may be considered biased.
But one thing patients are not clamoring for: Healthcare-related apps. Fewer than half of patients felt that a healthcare app would be a helpful tool for them. In fact, only 17% of patients reported that they “always” or “frequently” use their smartphone to help with healthcare. Of course, some patients said they couldn’t use an app because they didn’t even own a smartphone, while others cited varying privacy concerns.
But when they do use apps, the most common uses are for: Helping to prepare for doctor visits (59%); searching for information online (56%); setting up dosing reminders (35%); taking notes at doctor’s office (35%); and taking photos of symptoms (30%).
Just because patients aren’t thrilled with apps, doesn’t mean mobile still isn’t an important channel for reaching patients.
“We were surprised at how much mobile devices for health were actually used for accessing the Web via a browser rather than using apps,” explains Loew. “A lot of our members were more likely to use the browsers on their phones rather than dedicated apps for health related things.”
In fact, when it comes to accessing Inspire online, Loew says that a year ago, 20% of the visits came from someone using a tablet, 35% came from a mobile phone and 45% came from users on a desktop. Now, the desktop and mobile numbers flipped with 45% accessing Inspire via a mobile phone and 35% via a desktop. These numbers were also one of the leading factors behind Inspire’s recent redesign, which is now more optimized for mobile users.
The tools/materials that patients feel would be helpful for them to use with their physicians include an electronic, detailed symptom tracker (59%); access to online webinars or in-person conferences/speaker sessions (57%); support materials for friends/family members detailing the condition and its symptoms (47%); printed, detailed symptom tracker (42%); and tips/tactics addressing better ways to communicate with physicians (40%).
Growing Affordability Concerns
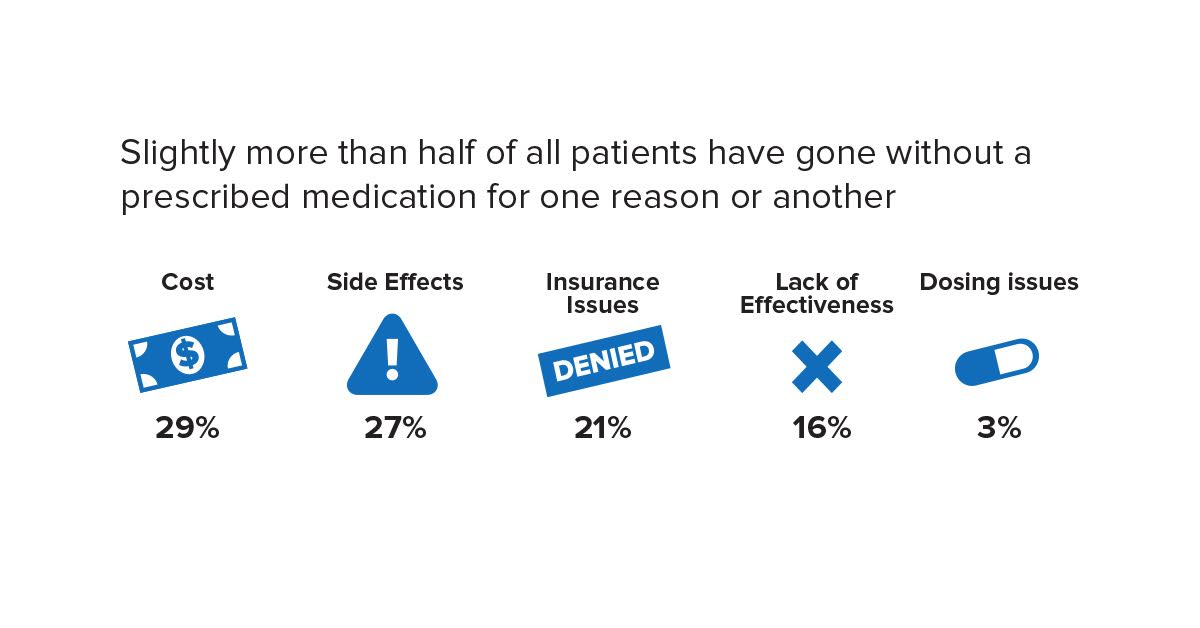
The most interesting aspect of the survey results, Loew says, concerned the affordability of healthcare.
Nearly two-thirds of patients (59%) had commercial insurance; 26% were on Medicare; 11% had state/country provided care; 9% had Medicaid, 8% stated “Other;” and 4% had coverage from the VA; while 4% had none. Still, patients faced financial difficulties across the board, including paying for treatment (60%); paying for other medications (56%); travel and logistics costs (47%); and cost of lab tests (29%). In terms of affording treatments, oncology patients were least likely to have difficulty, while neurology patients were most likely.
The survey included respondents from six continents, but patients in the U.S. felt the greatest impact on their insurance premiums (55% reported an increase), office co-pays (44%) and ancillary treatment costs (37%). Another 60% said at least one of their medications was switched by their insurance company to a generic equivalent—and some respondents even claimed this was done without any notification.
“It seems that when it comes to affording healthcare, it’s almost bifurcated in the sense that people either have problems with affordability or reimbursement, or they don’t,” explains Loew. “Many people might grumble a little about increasing co-pays or something like that, but they are basically fine. But others have big affordability problems and are unhappy. Not a huge amount are in the middle.”