AT ASBMR
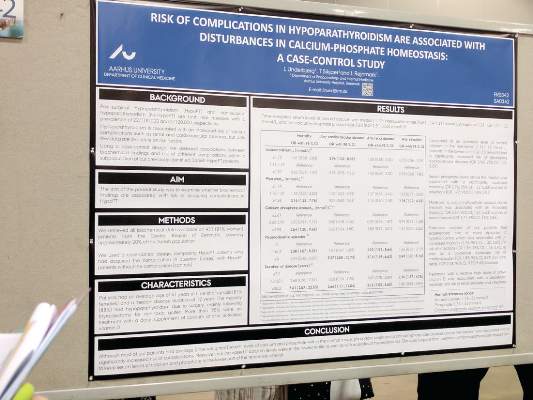
DENVER (FRONTLINE MEDICAL NEWS) – Most patients maintained time-weighted serum levels in the normal range in a case-control study of hypoparathyroidism, but serum levels of phosphate and calcium phosphate above median values were associated with a higher mortality and risk of complications.
Patients with calcium levels in the lowest tertile also had an increased risk of cardiovascular disease, while those who experienced episodes of hypercalcemia had a higher risk of mortality and infections.
The findings cannot prove causation, but they nevertheless suggest that physicians treating hypoparathyroidism should consider aiming to keep serum calcium and phosphate levels in the lower range of the reference interval, although all treatment decisions should be patient specific, according to Line Underbjerg, MD , of Aarhus (Denmark) University Hospital, who presented the study in a poster session at the annual meeting of the American Society for Bone and Mineral Research.
Denmark has a well-established cohort of patients with hypoparathyroidism, and previous epidemiologic studies have shown that those patients have increased risks of cardiovascular disease, renal diseases, and infections.
“From our epidemiologic study, we did not see increased mortality when we compared patients with hypoparathyroidism to [the] Danish population. So, we were actually a bit surprised that the phosphate and the calcium phosphate product had an influence on mortality,” said Dr. Underbjerg.
To find out if there were any associations between the biochemical findings and complications, the researchers collected biochemical data on 431 patients with hypoparathyroidism (81% of whom were women, with an average age of 41 years and a median disease duration of 12 years); 88% of the patients had the condition as a result of surgery, and 95% of patients received daily calcium and/or activated vitamin D supplements.
The researchers looked at four complications: mortality, cardiovascular disease, renal disease, and any infection. For each complication, they compared patients who had experienced the complication to hypoparathyroidism patients who did not experience the complication.
The subjects had a median time-weighted serum level of ionized calcium of 1.17 mmol/L (interquartile range [IQR], 1.14-1.21), a median of value of 1.21 mmol/L of phosphate (IQR, 1.11-1.32), and a median value of 2.80 mmol2/L2 of the calcium-phosphate product (IQR, 2.51-3.03).
Patients in the lowest tertile of ionized calcium (less than or equal to 1.16) had a greater risk of developing cardiovascular diseases than patients in the midtertile (1.16-1.19; odds ratio [OR], 2.96; 95% confidence interval [CI], 1.02-8.59).
Compared with patients in the midquartile, patients with serum phosphate levels above the median value of 1.21 were at a higher risk of mortality (OR, 2.76; 95% CI, 1.32-5.80) and infections (OR, 1.77; 95% CI, 1.04-3.01).
Calcium-phosphate product levels above the median value of 2.80 were associated with heightened mortality (OR, 2.67; 95% CI, 1.27-5.63) and renal diseases (OR, 1.71; 95% CI, 1.03-2.86).
Hypercalcemia occurred in 41% of patients and was also tied to increased mortality (OR, 1.76; 95% CI, 1.02-3.05) and risk of infections (OR, 1.86; 95% CI, 1.18-2.93).
The results suggest that those values have the potential to be clinically important. “I think you have to be aware that phosphate and calcium phosphate levels have an influence on a patient’s well-being,” said Dr. Underbjerg.
Shire funded the study. Dr. Underbjerg reported having no relevant financial disclosures.