PM360 asked for companies to send in their latest and best ways to improve adherence. Here are twelve of the best examples of programs, strategies, solutions, technology, and more that companies have developed or are using to keep patients on their prescribed therapies.
PSP+ Companion App
BrightInsight
Jamie Burgess, Senior Vice President, Marketing jamie.burgess@brightinsight.com
 Patient support programs (PSPs) are a proven way to smooth the patient journey, speed time to fill, and improve conversion. But outdated manual processes are complex and leave many patients out. Launched in April 2023, BrightInsight’s PSP+ Companion App, built on the compliant BrightInsight Platform, connects patients to the resources they need to complete prior authorization, register for financial assistance, understand and track their therapies, and much more. Features include custom hub and PSP integration so patients can track prior authorization status and communicate with payers and providers as well as exchange secure documents; configurable charts and graphs to illustrate trends and generate feedback to help patients understand the impact of their therapy, which can be shared with HCPs; configurable patient-centric tools such as at-home SubQ body map for infusion site tracking, in-app timer for temperature control, patient journal, and more to keep patients engaged; and custom educational material and PSP care team support. The PSP+ Companion App enables patients to administer their therapies properly for an optimal patient experience, ultimately improving adherence.
Patient support programs (PSPs) are a proven way to smooth the patient journey, speed time to fill, and improve conversion. But outdated manual processes are complex and leave many patients out. Launched in April 2023, BrightInsight’s PSP+ Companion App, built on the compliant BrightInsight Platform, connects patients to the resources they need to complete prior authorization, register for financial assistance, understand and track their therapies, and much more. Features include custom hub and PSP integration so patients can track prior authorization status and communicate with payers and providers as well as exchange secure documents; configurable charts and graphs to illustrate trends and generate feedback to help patients understand the impact of their therapy, which can be shared with HCPs; configurable patient-centric tools such as at-home SubQ body map for infusion site tracking, in-app timer for temperature control, patient journal, and more to keep patients engaged; and custom educational material and PSP care team support. The PSP+ Companion App enables patients to administer their therapies properly for an optimal patient experience, ultimately improving adherence.
Patient Engagement Solution
Courier Health
Andrew Sopko, Business Development Executive andrew@courierhealth.com  Courier Health is a New York-based technology company providing an innovative patient engagement solution for life sciences. Courier Health’s solution connects data from key partners (reimbursement, hubs, pharmacies, EHR, sales, and more) to create personalized patient journeys. Their solution is used by Marketing, Field Reimbursement, and Patient Services teams to ensure patients can successfully start and stay on therapy. With Courier Health, life sciences companies can design and orchestrate patient journeys that are coordinated across communication channels and key stakeholders. On average, 30% of patients who are prescribed a specialty therapy do not start treatment. Worse, about 50% of patients that start end up discontinuing in the first two to three months. The majority of these patients who never start or discontinue are often lost between disparate systems and manual processes. Courier Health addresses this issue by providing a central solution to visualize each step of the patient journey, identify friction points, and automate proactive resolution. For example, one of Courier Health’s clients uses patient engagement, insurance, refill, and other information to personalize their adherence program. Some patients require more support due to their insurance (e.g., re-auths), while others prefer text or email reminders over a Patient Services team member. Personalizing the patient experience has increased adherence by over 35% and enabled their Patient Support team to scale efficiently.
Courier Health is a New York-based technology company providing an innovative patient engagement solution for life sciences. Courier Health’s solution connects data from key partners (reimbursement, hubs, pharmacies, EHR, sales, and more) to create personalized patient journeys. Their solution is used by Marketing, Field Reimbursement, and Patient Services teams to ensure patients can successfully start and stay on therapy. With Courier Health, life sciences companies can design and orchestrate patient journeys that are coordinated across communication channels and key stakeholders. On average, 30% of patients who are prescribed a specialty therapy do not start treatment. Worse, about 50% of patients that start end up discontinuing in the first two to three months. The majority of these patients who never start or discontinue are often lost between disparate systems and manual processes. Courier Health addresses this issue by providing a central solution to visualize each step of the patient journey, identify friction points, and automate proactive resolution. For example, one of Courier Health’s clients uses patient engagement, insurance, refill, and other information to personalize their adherence program. Some patients require more support due to their insurance (e.g., re-auths), while others prefer text or email reminders over a Patient Services team member. Personalizing the patient experience has increased adherence by over 35% and enabled their Patient Support team to scale efficiently.
Rx Savings Program
Healthline Media
Elisabeth Paredes, VP of Sales eparedes@heathline.com 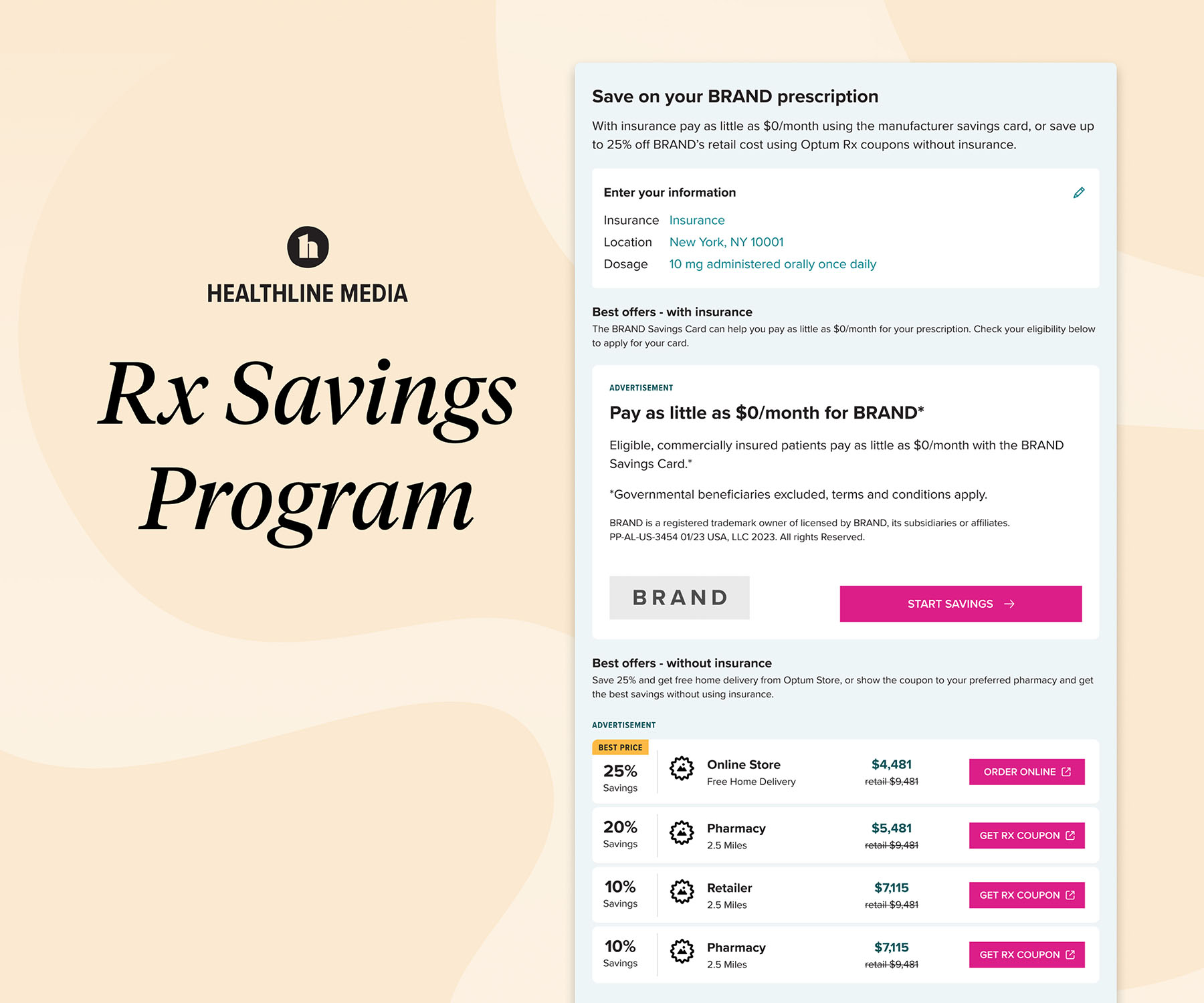 High drug prices routinely turn consumers away at the point of purchase. Nearly three in five people have experienced out-of-pocket prescription costs they couldn’t afford.1 Healthline Media’s new solution, Rx Savings Program, is an interactive experience on its drug information pages that drives users to take action with manufacturer drug savings programs, helping them better afford and adhere to treatment. The Rx Savings Program platform, which debuted in pilot form in February 2023 and became fully live in July, highlights actionable cost-saving opportunities for eligible consumers who are already researching treatment information and may be concerned about affordability. Knowing that three out of five health information seekers won’t visit a drug manufacturer’s site directly, this offering meets consumers where they are with information about and access to pharma brands’ manufacturer copay programs that are relevant to them.1 About half of the general U.S. population has never used an Rx discount service, and four in 10 of this group aren’t sure how it works or where to start.2 Through this interactive treatment savings experience, consumers have a clear path forward from the research stage to point of purchase. In fact, after learning about prescription medications on Healthline Media’s website, 69% of visitors say they are extremely or very likely to refill their current prescription.1 References: 1. Healthline Media Consumer Drug Information Pages Visitor survey. Feb-May 2022. 2. Healthline Media Rx Medication Discount Service survey. Dec 2022.
High drug prices routinely turn consumers away at the point of purchase. Nearly three in five people have experienced out-of-pocket prescription costs they couldn’t afford.1 Healthline Media’s new solution, Rx Savings Program, is an interactive experience on its drug information pages that drives users to take action with manufacturer drug savings programs, helping them better afford and adhere to treatment. The Rx Savings Program platform, which debuted in pilot form in February 2023 and became fully live in July, highlights actionable cost-saving opportunities for eligible consumers who are already researching treatment information and may be concerned about affordability. Knowing that three out of five health information seekers won’t visit a drug manufacturer’s site directly, this offering meets consumers where they are with information about and access to pharma brands’ manufacturer copay programs that are relevant to them.1 About half of the general U.S. population has never used an Rx discount service, and four in 10 of this group aren’t sure how it works or where to start.2 Through this interactive treatment savings experience, consumers have a clear path forward from the research stage to point of purchase. In fact, after learning about prescription medications on Healthline Media’s website, 69% of visitors say they are extremely or very likely to refill their current prescription.1 References: 1. Healthline Media Consumer Drug Information Pages Visitor survey. Feb-May 2022. 2. Healthline Media Rx Medication Discount Service survey. Dec 2022.
Alliance by Aspen RxHealth
Aspen RxHealth
Jennifer Cohen, Senior Vice President, Marketing & Communications jennc@aspenrxhealth.com As a company founded by pharmacists for pharmacists, Aspen RxHealth understands why medication adherence is so critically important. That’s why it uses technological innovation to empower pharmacists to provide direct consultative care and boost medication adherence. Alliance by Aspen RxHealth, which debuted in October 2022, is its latest solution. It allows health plans’ in-house pharmacy teams to utilize its proprietary platform and support services to complete pharmacy consultations for their member populations. Proactive adherence management is a vital aspect of these consultations to ensure that patients being treated for chronic conditions such as diabetes, hypertension, and cholesterol issues maintain medication adherence. Should a health plan’s capacity to complete consultations be insufficient, Aspen RxHealth’s gig-economy community of over 7,000 pharmacists is standing by, able to augment efforts and ensure all members receive the care they need without forsaking their experience. The platform automates the intelligent matching of members with pharmacists based on language, location, and pharmacist area of specialty to improve health outcomes. Once matching occurs, consultation opportunities are presented to pharmacists through an iOS application, and members receive a phone call from the pharmacist best attuned to their personal and medical background. As a result, health plans around the country using Alliance by Aspen RxHealth are lowering costs, increasing efficiencies, and keeping members healthier while leveraging their in-house pharmacy teams to conduct outreach.
THRiV
Adheris Health
Sen Deng, SVP Analytics sen.deng@adherishealth.com  For 30 years, Adheris Health has been solving medication adherence challenges and through this experience has gained a deep understanding of the factors influencing adherence. Over the last two years, the company deployed proprietary machine learning on hundreds of data points linking patients’ medications, histories, care support, and their relations with the prescribers. The results? Four actionable dimensions that drive individualized interventions to improve adherence. Launched in 2021, Adheris Health’s intelligent patient platform, THRiV, translates these patient insights into actions. Supported by the data of over 226 million patients, Adheris Health builds intricate models to create individual therapeutic risk scoring of medication complexity, adherence scoring of predicted behaviors, care burden from cycles of treatment and costs, and socioeconomic determinants surrounding the patient. Powered by these insights, interventions are designed into programs that are delivered where the patient needs them, when it is the best time to absorb new information, with curated resources as to what is most effective for adherence individually. The THRiV platform allows for proactive intervention with supporting resources when a patient interacts with their pharmacists in store, takes treatment at home, or engages digitally with text messages. By creating an omnichannel patient-centric experience, Adheris Health can support patients with a holistic approach to empower better health with individualized content such as medication education, use instructions, or financial assistance. Additionally, the company can assess its patient adherence and awareness programs by employing a control mechanism to accurately capture the impact of interventions on an immense patient population.
For 30 years, Adheris Health has been solving medication adherence challenges and through this experience has gained a deep understanding of the factors influencing adherence. Over the last two years, the company deployed proprietary machine learning on hundreds of data points linking patients’ medications, histories, care support, and their relations with the prescribers. The results? Four actionable dimensions that drive individualized interventions to improve adherence. Launched in 2021, Adheris Health’s intelligent patient platform, THRiV, translates these patient insights into actions. Supported by the data of over 226 million patients, Adheris Health builds intricate models to create individual therapeutic risk scoring of medication complexity, adherence scoring of predicted behaviors, care burden from cycles of treatment and costs, and socioeconomic determinants surrounding the patient. Powered by these insights, interventions are designed into programs that are delivered where the patient needs them, when it is the best time to absorb new information, with curated resources as to what is most effective for adherence individually. The THRiV platform allows for proactive intervention with supporting resources when a patient interacts with their pharmacists in store, takes treatment at home, or engages digitally with text messages. By creating an omnichannel patient-centric experience, Adheris Health can support patients with a holistic approach to empower better health with individualized content such as medication education, use instructions, or financial assistance. Additionally, the company can assess its patient adherence and awareness programs by employing a control mechanism to accurately capture the impact of interventions on an immense patient population.
Patient Access Service
Inizio Engage
Nareda Mills, Global President, Patient Solutions nareda.mills@inizio.com 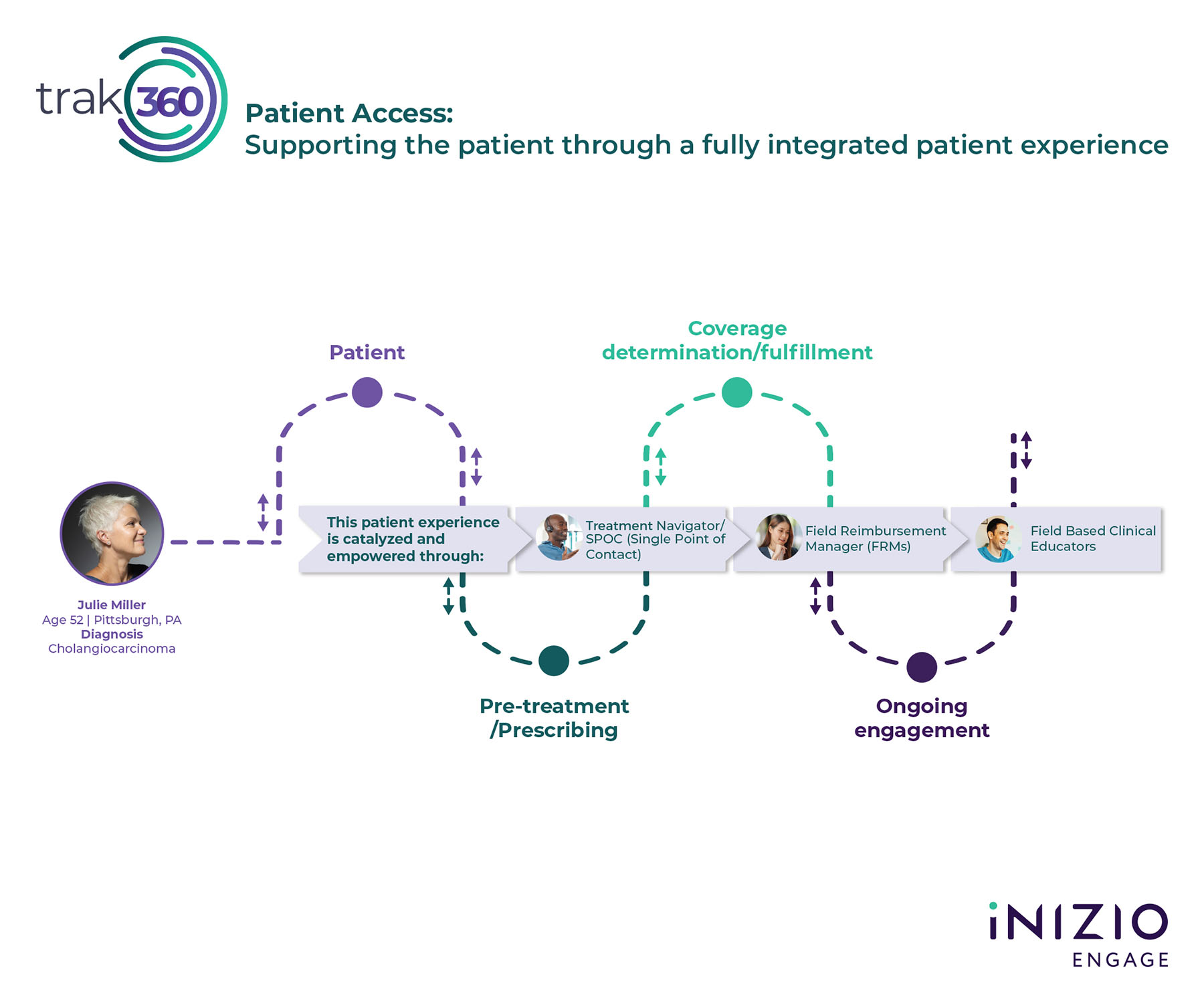 The Patient Access service from Inizio Engage, which launched in July 2023, bridges the patient support gap from medication access through adherence. Drawing upon the company’s 20 years of experience in patient support, Patient Access seeks to encourage adherence and improve outcomes by addressing the complexities patients must navigate post diagnosis to obtain and use treatment when diagnosed with a specialty or rare and orphan disease. Based upon years of client demand from Inizio Engage and its enriched Trak360 technology platform, Patient Access offers an expanded suite of services:
The Patient Access service from Inizio Engage, which launched in July 2023, bridges the patient support gap from medication access through adherence. Drawing upon the company’s 20 years of experience in patient support, Patient Access seeks to encourage adherence and improve outcomes by addressing the complexities patients must navigate post diagnosis to obtain and use treatment when diagnosed with a specialty or rare and orphan disease. Based upon years of client demand from Inizio Engage and its enriched Trak360 technology platform, Patient Access offers an expanded suite of services:
- Treatment Navigators who provide supplemental education on the disease, its treatment, possible side effects, and address patient concerns on the road ahead. They review the patient’s benefits, help to determine copay eligibility, work with the patient and their provider to obtain prior authorization when needed, and provide the educational support to the HCP practice for the appeal process if prior authorization is denied.
- Field Reimbursement Managers (FRMs) who educate HCP office staff on navigating patient enrollment to increase the speed to therapy by ensuring first submission excellence. Drawing upon a complex payer policy database, FRMs work to ensure prior authorizations are submitted with robust data and alignment with the required details, and then follow patient progress to coverage in real time.
- Clinical Educators who deliver top-tier supplemental disease education and treatment administration support, as well as behavioral health skill building and nutrition guidance to patients and their care partners. Support can be provided in-person and/or virtually. They also provide HCP education on the disease state, its treatment, and how to administer the treatment.
Reasons for Discontinuation (RfD) Analytics Report
OM1
Maria Demko, Senior Marketing Associate mdemko@om1.com  An estimated 50% of patients with a prescription for a chronic condition stop taking it within the first year, leading to worse outcomes and nearly $250 billion lost revenue annually for the pharmaceutical industry. To combat this, OM1 launched its Reasons for Discontinuation (RfD) Analytics Report in February 2023. The report contains highly valuable, difficult-to-obtain medication discontinuation trends; uncovering the leading causes of why patients stop taking their medications in primary dermatologic and rheumatologic conditions, including rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, and psoriasis. The model leverages an AI model predicated on a dataset that encompasses billions of data points from more than 300 million patients. Drug manufacturers know that patients are discontinuing their medications based on claims data but lack a clear understanding as to why; many companies have been dependent on physician recall and limited surveys to understand these reasons. Until now, these companies have not been able to uncover the reasons for discontinuation. The RfD Analytics Report directly extracts and categorizes these reasons from the clinical narrative at scale. In the end, the report provides actionable insights to inform brand strategy. With these insights, drug manufacturers can better understand patient and provider motivations around therapeutic discontinuation. The result is informed decisions to improve patient outcomes, patient engagement, and commercial performance. Ultimately, manufacturers gain insight into why patients and physicians stop a particular therapy, allowing for interventions related to tolerability, costs, and emerging contraindications.
An estimated 50% of patients with a prescription for a chronic condition stop taking it within the first year, leading to worse outcomes and nearly $250 billion lost revenue annually for the pharmaceutical industry. To combat this, OM1 launched its Reasons for Discontinuation (RfD) Analytics Report in February 2023. The report contains highly valuable, difficult-to-obtain medication discontinuation trends; uncovering the leading causes of why patients stop taking their medications in primary dermatologic and rheumatologic conditions, including rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, and psoriasis. The model leverages an AI model predicated on a dataset that encompasses billions of data points from more than 300 million patients. Drug manufacturers know that patients are discontinuing their medications based on claims data but lack a clear understanding as to why; many companies have been dependent on physician recall and limited surveys to understand these reasons. Until now, these companies have not been able to uncover the reasons for discontinuation. The RfD Analytics Report directly extracts and categorizes these reasons from the clinical narrative at scale. In the end, the report provides actionable insights to inform brand strategy. With these insights, drug manufacturers can better understand patient and provider motivations around therapeutic discontinuation. The result is informed decisions to improve patient outcomes, patient engagement, and commercial performance. Ultimately, manufacturers gain insight into why patients and physicians stop a particular therapy, allowing for interventions related to tolerability, costs, and emerging contraindications.
Factor My Way
Octapharma
Eric Marrero, Director, Brand Marketing and Communications eric.marrero@octapharma.com  Factor My Way is Octapharma’s support program for patients living with bleeding disorders. It is the first and only bilingual support program for patients with hemophilia A and von Willebrand disease, their caregivers, families, and friends. It was developed through close partnership with the community to meet their broad, diverse, and evolving needs. The program is uniquely tailored to what patients, caregivers, and HCPs identified as the resources to best support patients, and continues to evolve through community feedback. Four comprehensive program pillars help patients to find strength, support, and community:
Factor My Way is Octapharma’s support program for patients living with bleeding disorders. It is the first and only bilingual support program for patients with hemophilia A and von Willebrand disease, their caregivers, families, and friends. It was developed through close partnership with the community to meet their broad, diverse, and evolving needs. The program is uniquely tailored to what patients, caregivers, and HCPs identified as the resources to best support patients, and continues to evolve through community feedback. Four comprehensive program pillars help patients to find strength, support, and community:
- Factor My Way Connection allows patients to find others who have walked in their shoes by engaging with patient experience managers, patient educators, nurse educators, and a Facebook community.
- Factor My Way Events features live and on-demand events with special community guest speakers, patient educator programs, and nurse educator programs.
- Factor My Way Learning is an extensive library of patient stories, information about bleeding disorders and treatment, and tips for healthy living.
- Factor My Way Assistance includes a free trial program, compassionate use, copay reimbursement assistance, and a live support center.
In addition to Factor My Way, Octapharma has created customized patient support programs across its portfolio, such as IgCares. IgCares is a full-circle support program for patients with primary immunodeficiency featuring novel solutions like medical waste management and opportunities to direct charitable donations.
Breast Cancer Patient Program
IQVIA In Home Clinical Solutions
Michael Zilligen, General Manager, In-Home Clinical Solutions michael.zilligen@iqvia.com 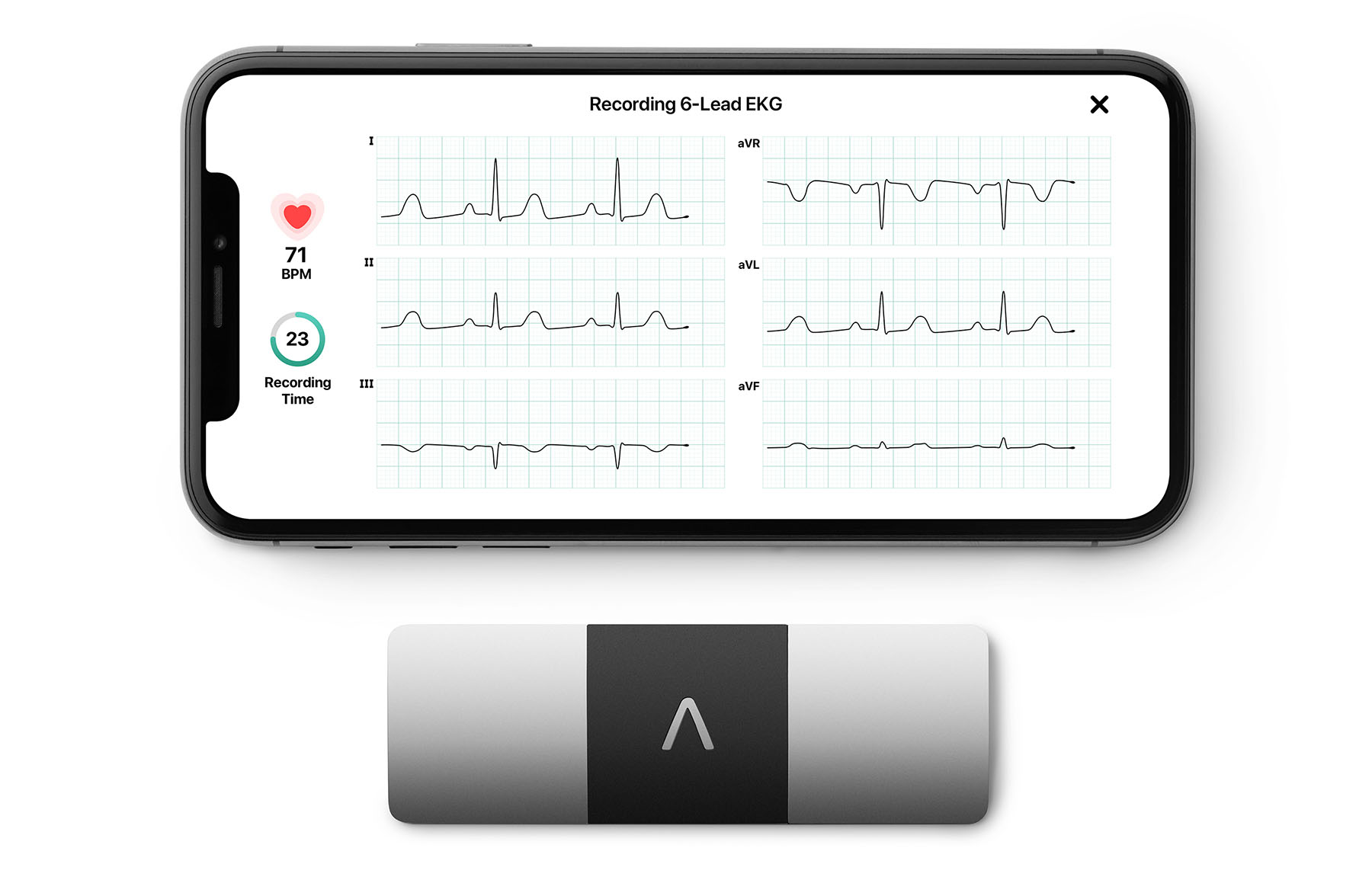 An increasing number of specialty therapies have unique patient safety and appropriate use criteria that require diagnostic tests and monitoring prior to patients being cleared for starting (or even staying on) treatment. Complicating matters further, patients who are candidates for a specialty therapy may struggle to start or stay on the prescribed treatment since they lack access to testing, have mobility challenges and do not want to burden their caregivers, and/or medical centers may have backlogs of several weeks for testing. The recent advancement of mobile technologies has become a tool that can be used to help patients and prescribers overcome challenges associated with required testing, such as in-home electrocardiograms (ECGs). Equipping patients and clinicians with state-of-the-art technology allows them the ability to complete the testing within the privacy and convenience of their own home. In 2021, IQVIA In Home Clinical Solutions pioneered an innovative program to address the challenge patients with breast cancer faced when trying to adhere to their treatment which required frequent ECG testing. Leveraging the elegant AliveCor 6L mobile ECG device (see image above), without leads like traditional equipment, these patients were provided a less invasive device which made it easier for them to take their own ECG. The program eliminated the need for the patients to travel to their oncologists’ offices, significantly increasing the group’s adherence to treatment.
An increasing number of specialty therapies have unique patient safety and appropriate use criteria that require diagnostic tests and monitoring prior to patients being cleared for starting (or even staying on) treatment. Complicating matters further, patients who are candidates for a specialty therapy may struggle to start or stay on the prescribed treatment since they lack access to testing, have mobility challenges and do not want to burden their caregivers, and/or medical centers may have backlogs of several weeks for testing. The recent advancement of mobile technologies has become a tool that can be used to help patients and prescribers overcome challenges associated with required testing, such as in-home electrocardiograms (ECGs). Equipping patients and clinicians with state-of-the-art technology allows them the ability to complete the testing within the privacy and convenience of their own home. In 2021, IQVIA In Home Clinical Solutions pioneered an innovative program to address the challenge patients with breast cancer faced when trying to adhere to their treatment which required frequent ECG testing. Leveraging the elegant AliveCor 6L mobile ECG device (see image above), without leads like traditional equipment, these patients were provided a less invasive device which made it easier for them to take their own ECG. The program eliminated the need for the patients to travel to their oncologists’ offices, significantly increasing the group’s adherence to treatment.
UltraTouch Verify
D2
Jim Maguire, Chief Information Officer jim.maguire@d2rx.com 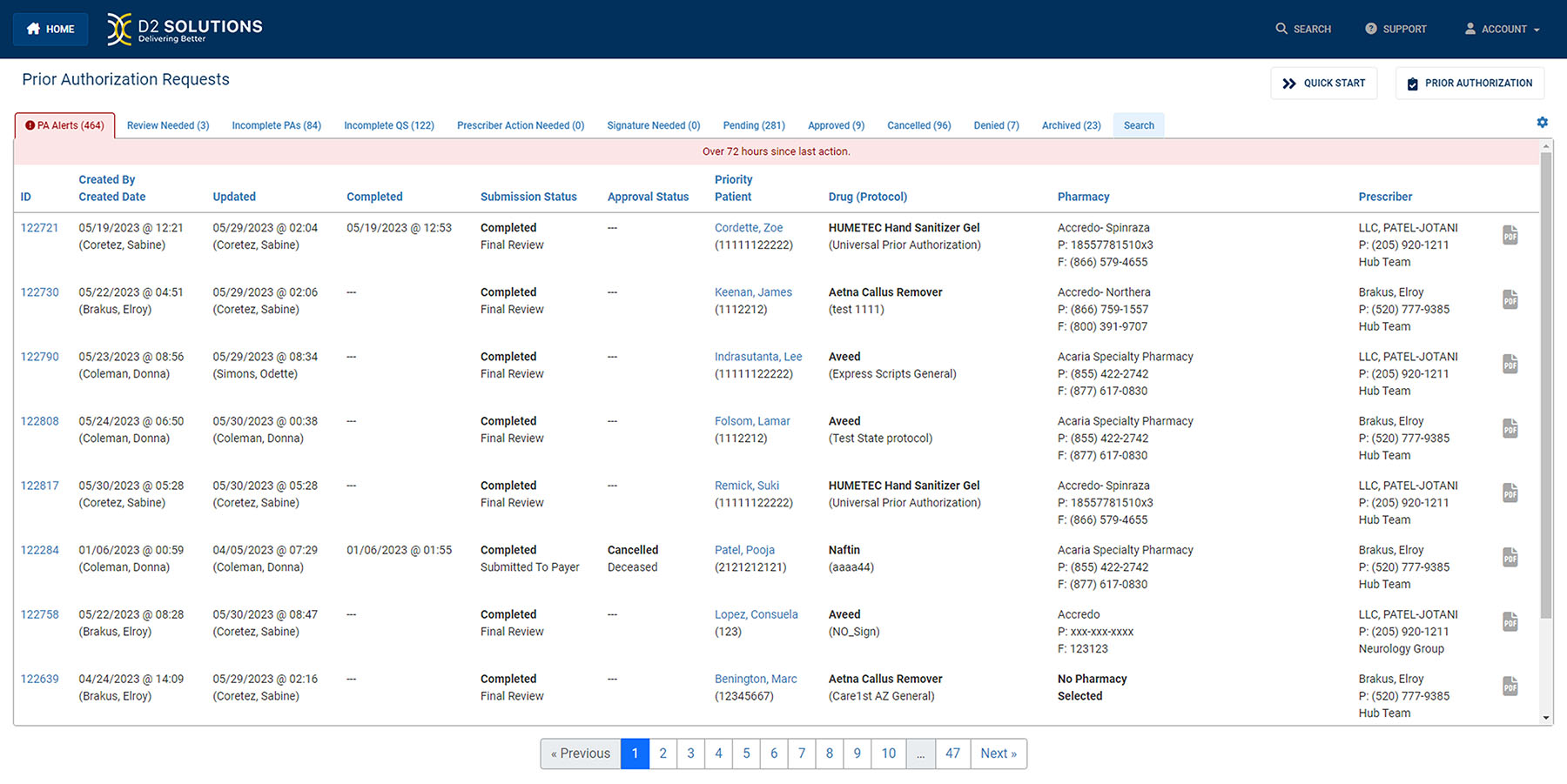 In 2022, D2 introduced UltraTouch Verify a SaaS solution developed in conjunction with its clients to address the needs of patients on specialty medications. Using gaming technology, this tool enables real-time enrollment via a QR code into programs including but not limited to Specialty Pharmacy Support, Clinical Management, and/or Reimbursement support. By enabling enrollment in real time, at the physician’s office, the patient is immediately aware of the program and the importance of it to the management of their healthcare journey. Results include:
In 2022, D2 introduced UltraTouch Verify a SaaS solution developed in conjunction with its clients to address the needs of patients on specialty medications. Using gaming technology, this tool enables real-time enrollment via a QR code into programs including but not limited to Specialty Pharmacy Support, Clinical Management, and/or Reimbursement support. By enabling enrollment in real time, at the physician’s office, the patient is immediately aware of the program and the importance of it to the management of their healthcare journey. Results include:
- Zero patients discontinued therapy when enrolled in the UltraTouch program.
- Leveraging the QR code enrollment process; there were no patients who were not able to be reached using digital outreach.
- 68% of the patients enrolled via the QR code chose to schedule a Welcome Call.
- Of the 68% who scheduled a Welcome Call, 61% answered the call on the first ring by knowing when they were going to be called. (Previously, only 15-18% of patients were answering the call and it typically took an average of five calls to reach a patient.)
- 85% of patients who enrolled in the UltraTouch program provide additional required information (e.g., insurance information, etc.) via digital submission, allowing workflows to proceed quicker, accelerating the patient onboarding process.
In fact, by allowing patients to respond digitally to requests for additional required information, the program was able to capture insurance information prior to the January 1st renewal, saving significant staff workload and streamlining the January re-enrollment process.
MEMS Mobile
AARDEX
Gemma Telfer, Marketing Lead gemma.telfer@aardexgroup.com 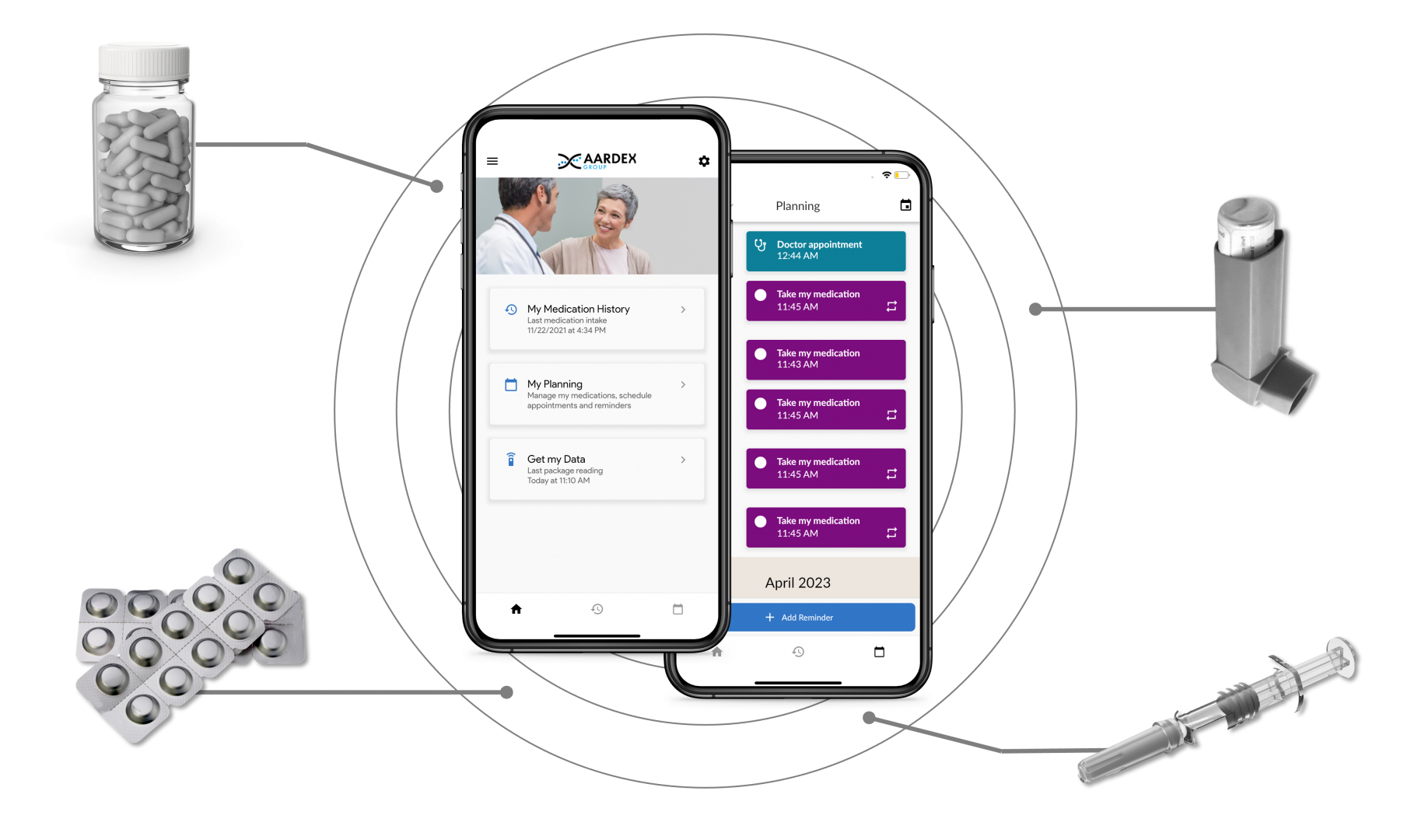 MEMS Mobile, which launched in 2021, is the latest addition to AARDEX’s ecosystem of advanced adherence solutions. The patient-facing app provides clinical trial participants with medication reminders and alerts, simplifying medication management, enhancing engagement to the protocol, and reducing the risk of missed doses. But this is no ordinary reminder service. Dosing data is also transmitted to MEMS AS, AARDEX’s real-time medication software. Powerful, proprietary analytics algorithms analyze the data to flag erratic or concerning patterns in medicine taking behavior. This provides researchers with insights into adherence at the study, site, and patient level, enabling them to identify any issues or concerns and take appropriate action, in the form of tailored, personalized interventions, quickly. In 2021, MEMS Mobile was used alongside a chatbot designed to deliver automatic adherence interventions, based on medication taking behavior data collected within the app. In a post-study survey, participants gave the app a system usability score (SUS) of between zero and 40. Of the 16 people who replied, 15 gave it a SUS of between 25 and 38. Satisfaction with the app was measured via CSQ-8, on a scale of between eight and 32. Ten people rated it as between 20 and 28, and five as between 17 and 20. Another ongoing study examined the impact of the app when used with the MEMS Button, a digitally enabled device patients use to record doses in real time with just one “click.” Of the 15 people involved in the study, 11 reported a drop in treatment-related anxiety after three months of using the approach.
MEMS Mobile, which launched in 2021, is the latest addition to AARDEX’s ecosystem of advanced adherence solutions. The patient-facing app provides clinical trial participants with medication reminders and alerts, simplifying medication management, enhancing engagement to the protocol, and reducing the risk of missed doses. But this is no ordinary reminder service. Dosing data is also transmitted to MEMS AS, AARDEX’s real-time medication software. Powerful, proprietary analytics algorithms analyze the data to flag erratic or concerning patterns in medicine taking behavior. This provides researchers with insights into adherence at the study, site, and patient level, enabling them to identify any issues or concerns and take appropriate action, in the form of tailored, personalized interventions, quickly. In 2021, MEMS Mobile was used alongside a chatbot designed to deliver automatic adherence interventions, based on medication taking behavior data collected within the app. In a post-study survey, participants gave the app a system usability score (SUS) of between zero and 40. Of the 16 people who replied, 15 gave it a SUS of between 25 and 38. Satisfaction with the app was measured via CSQ-8, on a scale of between eight and 32. Ten people rated it as between 20 and 28, and five as between 17 and 20. Another ongoing study examined the impact of the app when used with the MEMS Button, a digitally enabled device patients use to record doses in real time with just one “click.” Of the 15 people involved in the study, 11 reported a drop in treatment-related anxiety after three months of using the approach.
The CodeBroker Health Platform
CodeBroker
Dan Slavin, CEO dan.slavin@codebroker.com  CodeBroker, a leader in e-couponing solutions for some of the largest national retailers, launched a proprietary technology platform designed for pharma in mid-2021. This novel mobile platform, focused on driving conversion and adherence, offers three core solutions:
CodeBroker, a leader in e-couponing solutions for some of the largest national retailers, launched a proprietary technology platform designed for pharma in mid-2021. This novel mobile platform, focused on driving conversion and adherence, offers three core solutions:
- Digital voucher, a modern alternative to traditional sampling
- Copay registration, patient retention, and analytics
- Connected surveying and insights
The CodeBroker platform addresses key adherence challenges common for pharmaceutical marketing and patient support services teams: having early visibility into refill gaps and risks of nonadherence, being able to track the patient longitudinally over time with real-time interception ability, finding an easy digital mechanism to share important patient experience insights with the HCP right upon the patient receiving/taking medication, and more. The CodeBroker solution can help improve adherence through a seamless customer experience that drives ongoing patient utilization, the leveraging of actionable early and ongoing product experience insights, real-time tracking by individual patient of program utilization data from sample/voucher/bridge through to paying patient conversion and continuing Rx, and advanced activity monitoring and reporting. Today, 92% of patients state they are more likely to use their medication copay card if it is available on their mobile device and nearly 50% felt the current process to obtain their copay card was cumbersome, according to a May 2023 CodeBroker patient survey. CodeBroker has demonstrated that its solution decreased the average time between scheduled fills by 10%, increased NRx’s by 35%, and provided actionable visibility and insights at each core stage of the patient journey for brands.







