FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Deep infiltrating endometriosis lesions were found to harbor several genetic mutations, including well-known cancer-driver mutations in the ARID1A, PIK3CA, KRAS, and PPP2R1A genes, investigators reported in the May 11 issue of the New England Journal of Medicine.
This finding was possible only through the use of a combination of next-generation sequencing tools, together with highly sensitive digital genomic assays. A finding of cancer-related mutations in noncancerous lesions – and, “in particular, in nonovarian deep infiltrating lesions that rarely (if ever) transform into cancer” – was very “surprising” and raises new questions about the pathobiology of endometriosis, said Michael S. Anglesio , PhD, of the University of British Columbia, Vancouver, and his associates.
Deep infiltrating endometriosis, one of three anatomical subtypes of the disorder, is characterized by nodules that locally invade pelvic structures such as the bowel or peritoneal wall to a depth of greater than 5 mm. The lesions include both epithelial and stromal components.
All three subtypes of endometriosis exhibit “benign clinical behavior and normal-appearing histologic features,” and are considered to be nonmalignant inflammatory lesions, Dr. Anglesio and his associates said. However, they also “recapitulate some features of malignant neoplasms, including local invasion and resistance to apoptosis,” the investigators noted.
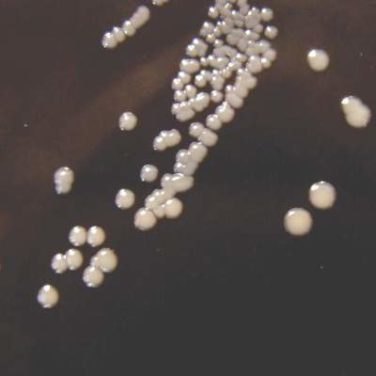
To further explore whether deep infiltrating endometriosis lesions harbor somatic mutations, they performed a series of genetic analyses on samples obtained from three independent cohorts of 27 affected patients in New York, Japan, and Vancouver. Whole-exome sequencing of lesions and adjacent normal tissue from 24 women revealed 80 different somatic mutations in 19 (79%) of the lesions.
The number of mutations per lesion varied widely, from 0 to 17, with a mean of 3.3 mutations per lesion. Five of these lesions harbored mutations in the cancer-driver genes ARID1A, PIK3CA, KRAS, or PPP2R1A.
In targeted-sequencing analyses of samples from three more patients, more activating mutations in the KRAS gene were found in two (66%). One woman had two different activating KRAS mutations, and the other had the same KRAS mutation in three separate lesions.
A further analysis of samples from an additional 12 patients showed KRAS mutations in 3 (25%) of them.
The data indicate that these mutations were very unlikely to have arisen by chance alone. In addition, “because cancer-driver mutations were present only in the epithelium but not the stroma of the same endometriosis lesion, we can assume that the observed mutations provide some key selective advantage to endometriotic epithelial cells,” Dr. Anglesio and his associates said (N Engl J Med. 2017 May 11. doi: 10.1056/NEJMoa1614814 ).
Their findings are consistent with those of recent studies of other organ systems, which reported cancer-driver mutations in benign lesions and in normal tissues from skin, neuronal, and ovarian samples, they added.
“Our findings challenge the current understanding of this invasive subtype of endometriosis and open the discussion on whether deep infiltrating endometriosis can be considered as a benign neoplasm,” the investigators wrote.
This study was sponsored by 27 nonindustry sources, including the Johns Hopkins University, the Virginia and D.K. Ludwig Fund for Cancer Research, the Ephraim and Wilma Shaw Roseman Foundation, the Endometriosis Foundation of America, and the National Institutes of Health. Dr. Anglesio reported having no relevant financial disclosures; some of his associates reported ties to several industry sources.