FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery ( 2016;151:1251-9 ).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
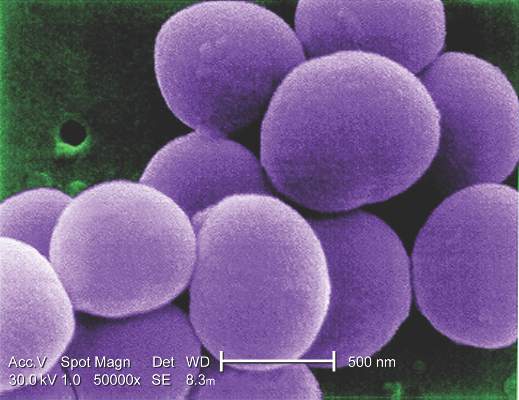
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue ( PLoS One. 2014;9:e112679 ; Transfus Med Hemother. 2011;38:379-86 ).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.