AT OBESITY WEEK 2017
NATIONAL HARBOR, MD. (FRONTLINE MEDICAL NEWS) – When combined with bariatric surgery, adjunctive therapies for obesity should be individualized for specific drivers of weight gain, which can differ among obesity phenotypes, according to an expert view presented at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society .
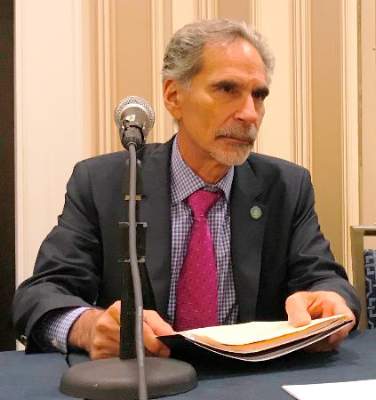
“Surgery is the most effective therapy we have, but it is only one of multiple treatments that should be considered in a treatment paradigm,” suggested Robert F. Kushner, MD , a professor of endocrinology and specialist in obesity at the Northwestern University, Chicago.
The remarks were part of a symposium in which Dr. Kushner was asked how surgeons should bridge the gap with nonsurgeon physicians working to improve outcomes in patients with obesity. Perhaps the most important point stressed by Dr. Kushner is that surgeons need to consider the obesity phenotype to understand what – in addition to surgery – will improve long-term outcomes.
“It is very useful to take a narrative approach to understand the patients in front of us and to understand who they are and how they got to where they are now,” Dr. Kushner explained. Dr. Kushner often asks patients to graph weight history over time. This can connect social, biological, and psychological events with significant weight gains, and these connections can generate insight into the underlying obesity phenotype.
“It is a like a fingerprint. Everyone has his or her own story to tell,” Dr. Kushner explained. A clinical picture of patients’ phenotypes can be developed from observing large jumps in weight connected to such factors as a stressful life event, a period of sustained inactivity, or a pregnancy. Over a weight history, several events may be identified that provide insight into each patient’s “unique weight journey.”
This understanding provides the basis for a systematic approach to combining strategies that may include lifestyle changes, surgery, and pharmacologic management, all tailored for the specific triggers and needs of the patient. Dr. Kushner advised that, even for those who are candidates for surgery, bariatric procedures are just one component of the treatment and must be integrated in a team approach with other modalities.
This approach may include pharmacologic therapy both before and after surgery; Dr. Kushner noted that the availability of drug options has expanded in recent years with approval of such therapies as lorcaserin and liraglutide. According to Dr. Kushner, drug therapy can be used for preoperative weight loss and may be useful for preventing postoperative weight gain in certain patients.
“There are no randomized trials demonstrating efficacy for prevention of postoperative weight gain, but there is supportive evidence from a retrospective study,” said Dr. Kushner, referring to a recently published two-center evaluation ( Surg Obes Relat Dis. 2017;13:491-500 ).
In that study, 258 patients underwent Roux-en-Y gastric bypass, and 61 patients underwent sleeve gastrectomy. Those who received adjunctive drug support, particularly in the RYGB group, had greater sustained weight loss than those who did not, leading to the conclusion that postoperative pharmacotherapy “is a useful adjunct.” The advantage for drug therapy was observed even though patients did not receive the most recently approved and potentially more effective drugs, according to Dr. Kushner. However, he cautioned that information about the optimal timing of treatment after surgery remains “limited.”
The variability in weight loss and weight regain after bariatric procedures is one reason to consider bariatric surgery as only one component in a continuum of care, according to Dr. Kushner. He emphasized that obesity is a chronic condition that requires ongoing and perhaps indefinite treatment. While surgeons may already work with a team that manages preoperative and postoperative lifestyle changes to improve immediate surgical outcomes, Dr. Kushner believes that surgeons and physicians should work more collaboratively toward long-term management plans. By also appreciating obesity phenotypes and the specific mix of treatments that are most likely to help individual patients achieve durable weight loss, surgeons and physicians working together are likely to improve outcomes beyond those that could be expected from either working alone.
Dr. Kushner reports he has financial relationships with Novo Nordisk, Retrofit, Takeda Pharmaceuticals, and Vivus.