EXPERT ANALYSIS FROM OARSI 2015
SEATTLE (FRONTLINE MEDICAL NEWS) – The pain of knee osteoarthritis is not exacerbated by regular exercise such as walking and may actually be relieved by it, according to several findings presented at the World Congress on Osteoarthritis.
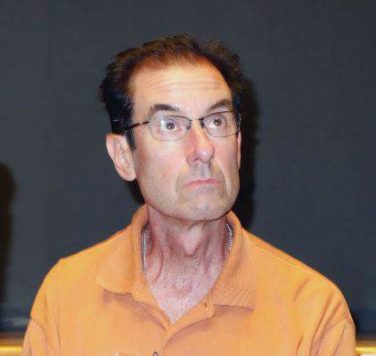
“Physical activity is important for the reduction of knee pain and the prevention of functional limitation in knee osteoarthritis,” Daniel White, Sc.D., said.
“We should be recommending walking to people with painful knee osteoarthritis. Just as a preliminary goal, we can start with 3,000 steps per day and ultimately progress people to at least 6,000 steps per day,” he added.
National guidelines issued in 2008 for the general population call for at least 150 minutes per week of moderate to vigorous–intensity physical activity, according to Dr. White of the department of physical therapy at the University of Delaware in Newark. When that recommendation is applied to walking, which is the most common physical activity among older adults ( Arthritis Care Res. 2014;66:139-46 ), it translates to a brisk pace that permits conversation but is exertional enough to cause sweating. Meeting the goal would mean approximately 100 steps per minute ( Am. J. Prev. Med. 2009;36:410-5 ).
“The clinical hypothesis is that osteoarthritis pain is limiting your physical activity, but whether that has been empirically [established] has yet to be seen,” Dr. White said. For example, investigators for an Osteoarthritis Initiative study found that only 13% of men and 8% of women with knee osteoarthritis met the criteria for the national guideline ( Arthritis Rheum. 2011;63:3372-82 ), but also noted that these values differed little from those of the general population. Data from the Multicenter Osteoarthritis Study found similarly low proportions, regardless of the presence of radiographic disease and the severity of knee pain ( Arthritis Rheum. 2013;65:139-47 ). In a cohort that underwent total knee replacement, patients had more than 180% improvements in subjective pain and function at 6 months, yet their objectively measured time spent walking increased by only 5% ( Clin. Orthop. Relat. Res. 2008;466:2201-8 ).
These findings suggest that osteoarthritis and pain may have a limited role in explaining physical inactivity, according to Dr. White. “An implication of this is that improvements in disease and pain may not lead to more physical activity; in other words, the pills you give to people to make them feel better or the exercises that they may do to improve their knee pain may not necessarily increase the amount of unstructured physical activity that people do on a day-to-day basis. Also, physical activity specifically may need to be targeted; you need to increase physical activity in a specific way rather than just expecting it to happen once the barriers of pain and disease are removed.”
Recommendations for physical activity must consider both potential risks and benefits, he noted. Data regarding its impact on structural changes in the knee are mixed. Conversely, there is substantial evidence that physical activity moderately reduces knee pain ( Cochrane Database Syst Rev. 2015;1:CD004376 ) and lowers the likelihood of developing functional limitations in a dose-response manner ( Arthritis Care Res. 2014;66:1328-36 ). And there are a variety of other health benefits, some of which may affect osteoarthritis, such as weight maintenance.
“In my mind, the benefits outweigh the risks for promoting physical activity in this patient population. And specifically, given that walking is the most common physical activity, from a clinical perspective, there is very strong evidence to recommend walking to this patient population,” Dr. White said at the meeting sponsored by the Osteoarthritis Research Society International.
He further endorsed use of a pedometer as a practical, objective way to measure this activity. “Regardless of what instrument or device you use, they all measure steps, and that is sort of the common denominator which is a very understandable outcome that patients can relate to, that clinicians understand,” he elaborated. Moreover, a meta-analysis has shown that interventions using pedometers achieve greater increases in walking ( JAMA 2007;298:2296-304 ).
The above analysis of impact on functional limitations in people with knee osteoarthritis also helps to define target walking goals, according to Dr. White, who disclosed that he had no relevant conflicts of interest. The study showed that 95% of people who did not develop functional limitations walked at least 3,000 steps per day, and that 6,000 steps per day best discriminated between those who did and did not develop functional limitations.
Assuming that a moderate intensity of walking is 100 steps per minute, this step range translates to 30-60 minutes of walking per day, he said. As half of 60-year-olds in the general population already walk approximately 40-50 minutes daily as part of their usual activities ( J. Gerontol. A Biol. Sci. Med. Sci. 2013;68:1426-32 ), they may need to add only 10 more minutes. And a recent report suggests that even people with severe knee osteoarthritis find this amount to be safe and feasible ( Osteoarthritis Cartilage 2015 April 14 [doi:10.1016/j.joca.2015.04.001] ).
rhnews@frontlinemedcom.com