AT SID 2017
PORTLAND, ORE. (FRONTLINE MEDICAL NEWS) – New research has uncovered “a new kid on the block” of genes underlying epidermolysis bullosa simplex (EBS), which may someday pave the way for new therapies, John McGrath, MD, said at the annual meeting of the Society for Investigative Dermatology.
The gene encodes kelch-like family member 24 (KLHL24), the substrate receptor of cullin 3-RBX1-KLHL24 complex, explained Dr. McGrath, professor of molecular dermatology, St. John’s Institute of Dermatology, King’s College London, where he studies heritable skin diseases. Keratin 14 is the substrate of this complex. In EBS, KLHL24 mutations affect methionine initiation codons, resulting in the loss of the first 28 amino acids of KLHL24 protein. As a result, the protein becomes overly stable, which leads to excessive ubiquitination and breakdown of keratin 14.
The end result is keratinocyte and skin fragility, Dr. McGrath said. “Clinically, these patients have quite a lot of birth trauma and generalized blistering. Somewhat unusual for EBS, you can also find nail abnormalities,” in addition to a pattern of atrophic scarring, he noted. As with many types of EBS, patients tend to spontaneously improve with age, but skin fragility persists, he added.
KLHL24 is the 19th gene to be implicated in EBS. News of the finding broke in late 2016, when two publications identified KLHL24 mutations in 19 patients with EBS from 10 different families. The first study, conducted in China, identified start-codon mutations in the KLHL24 gene in five patients, confirmed keratin 14 as the substrate of the protein, and established that KLHL24 mutations induce disproportionate ubiquitination and fragmentation of keratin 14. The researchers confirmed these results by using a knock-in mouse model ( Nat Genet. 2016 Dec;48 [12]:1508-16).
Meanwhile, European researchers identified KLHL24 mutations in families from Israel, Germany, Switzerland, Finland, Qatar, and Italy, and confirmed that these mutations affect the equilibrium between intermediate keratin filaments and keratin breakdown that is necessary for skin integrity ( Am J Hum Genet. 2016 Dec 1;99[6]:1395-1404 ).
EBS affects more than 400,000 individuals worldwide, and is usually linked to heterozygous missense mutations in genes encoding keratins 5 and 14, Dr. McGrath noted. “However, EBS is clinically and genetically heterogeneous,” he added. “About 20% of cases have no mutation in known genes.” Pursuing an accurate diagnosis of EBS subtype is important for genetic counseling and clinical care, he emphasized.
Therefore, to help confirm the findings of the studies in China and Europe, Dr. McGrath and his associates performed Sanger sequencing, skin pathology, clinical phenotyping, and electron microscopy of samples from undiagnosed cases of EB simplex that were banked at the U.K.’s National Diagnostic EB Laboratory . Among 183 cases (about 20% of all EBS referrals to the laboratory) that had not been linked to other mutations, 7 from six families had heterozygous KLHL24 mutations.
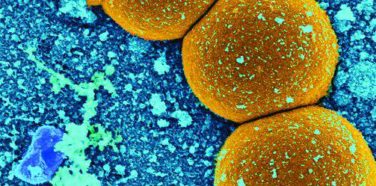
Together, the three studies name five KLHL24 mutations from 26 individuals, 16 families, and eight countries, Dr. McGrath said. “All these mutations target the initiation codon of methionine,” he added. As has previously been reported in EBS, immunostaining for keratin 14 is positive, outlining areas of cleavage within the basal cell layer of the skin. Semi-thin sections reveal pallor in the basal layer of keratinocytes, and electron microscopy of this layer shows blister formation.
“In nonlesional basal keratinocytes, there are few keratin filaments and mitochondria are prominent,” Dr. McGrath explained. “Higher magnification confirms the lack of identifiable keratin filaments, and reveals prominent microtubules.” Lesional skin shows not only the paucity of keratin filaments, but clear evidence of cytolysis, with numerous autophagosomes, autolysosomes, and disruption of organelles in the cellular cytoplasm. “The keratin has been chopped up, digested, and is being organically recycled. That’s essentially what’s going on here,” he said.
These studies show how clinician scientists can help advance the diagnosis and treatment of skin diseases by linking clinical and molecular pathology, Dr. McGrath said. But just as importantly, they might reveal a new approach to treating EBS. “Instead of gene editing or protein therapy, we have a new mechanism that may be ripe for proteasomal inhibitors or other targets of the ubiquitination pathway,” he added. “It’s an intriguing way forward when thinking about drugs and small molecules for EB therapy.”
The National Institute for Health Research and the NHS Foundation Trust funded the study. Dr. McGrath had no relevant financial disclosures.