FROM THE LANCET
Phase 3 data with siponimod, Novartis’ investigational treatment for multiple sclerosis, show a 21% reduction in the time to disease progression versus placebo in patients with the secondary progressive subtype of the disease.
A significantly lower percentage of patients with secondary progressive multiple sclerosis (SPMS) treated with siponimod met the primary endpoint of confirmed disease progression (CDP) at 3 months, compared with those who received placebo in the EXPAND trial (26% vs. 32% of patients; hazard ratio [HR], 0.79; 95% confidence interval [CI], 0.65–0.95; P = .013).
“The siponimod EXPAND study is, to our knowledge, the first large trial of any disease-modifying therapy to show superiority over placebo in terms of disability progression in a representative population of patients with SPMS,” lead author Ludwig Kappos of University Hospital, University of Basel (Switzerland), and his coinvestigators reported online March 22 in The Lancet . The study population involved “a large proportion of patients who had reached the non-relapsing stage of SPMS and had a high level of established disability,” they observed.
No significant difference between siponimod and placebo was seen in one of the two main secondary outcomes of the study – the time to 3-month confirmed worsening of the timed 25-foot walk test (T25FW). This result led Luanne Metz , MD, and Wei-Qiao Liu, MD, both of the department of clinical neurosciences and the Hotchkiss Brain Institute at the University of Calgary (Alta.), to take a cautionary view of the findings in an editorial about the trial’s results.
“Although siponimod seems to reduce the time to confirmed disability in SPMS, the treatment effect was small,” Dr. Metz and Dr. Liu argued.
“In our opinion, the reduction in the proportion of participants reaching the primary endpoint of only 6% and the absence of a significant difference for the key secondary clinical outcome [T25FW] are disappointing results and do not suggest that siponimod is an effective treatment for SPMS,” the two wrote.
“Confidence in the treatment benefit of siponimod in progressive MS will, in our opinion, require confirmation in a second trial. Trials of other novel treatments that target noninflammatory mechanisms are still needed,” they said.
EXPAND (Exploring the efficacy and safety of siponimod in patients with secondary progressive multiple sclerosis) was an event- and exposure-driven double-blind trial that recruited patients with SPMS over a 2-year period starting in February 2013. Of 1,651 patients who were recruited, randomized, and actually received treatment, 1,099 were treated with oral siponimod, 2 mg once daily, and 546 were given a matching placebo.
Treatment was for up to 3 years or until 374 CDP events assessed via the Expanded Disability Status Scale (EDSS) had occurred. Patients who had CDP after 6 months in the double-blind trial could be re-consented and continue with double-blind treatment, switch to open-label siponimod, or stop study treatment and either remain on no treatment or receive another disease-modifying treatment.
On average, the patients had been diagnosed with SPMS for a mean of 3.8 years and had been first diagnosed with MS around 17 years prior to this.
The primary endpoint of the trial – CDP at 3 months – was first reported in 2016 at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS). CDP was defined as a 0.5- to 1-point increase in EDSS depending on the baseline score.
A host of additional secondary endpoints were studied, with the risk of 6-month CDP being significantly reduced by siponimod versus placebo (HR, 0.74; 95% CI, 0.60-0.92; P = .0058).
The change from baseline in T2 lesion volume – the second of the two main secondary endpoints studied – showed a potential benefit of siponimod treatment over placebo, with a lower mean-adjusted increase in lesion volume over months 12 and 24 (183.9 mm3 vs. 879.2 mm3; P less than .0001).
More patients receiving siponimod than placebo were free from new or enlarging T2 lesions (57% vs. 37%) or T1 gadolinium-enhancing lesions (89% vs. 67%), and brain volume decreased at a lower rate with siponimod than with placebo.
Adverse events occurred at a higher rate with siponimod than with placebo (89% of patients vs. 82%), of which 18% and 15%, respectively, were defined as serious.
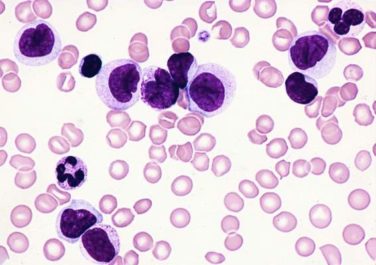
Adverse events seen more commonly in siponimod- than in placebo-treated patients were lymphopenia (1% vs. 0%), abnormal liver-related investigations (12% vs. 4%), hypertension (10% vs. 8%), and bradycardia (4% vs. 3%) and bradyarrhythmia (3% vs. 0.4%) at the start of treatment, which were mitigated by dose titration. Other adverse events that occurred less often but more frequently with siponimod included macular edema (2% vs. less than 1%), reactivation of varicella zoster (2% vs. 1%), and convulsions (2% vs. less than 1%).
“The safety profile of siponimod in EXPAND was generally aligned with that of other drugs in the class,” Dr. Kappos and his colleagues observed.
Siponimod, also known as BAF312, is a selective sphingosine 1-phosphate (S1P) receptor modulator that targets the targets the S1P 1 and 5 receptor subtypes; the other currently approved drug in its class is fingolimod (Gilenya), which is currently indicated for treating the relapsing-remitting form of multiple sclerosis (RRMS).
Phase 2 data have shown that siponimod could also be a promising treatment for RRMS, with reduced relapse rates and fewer brain lesions seen versus placebo ( JAMA Neurol. 2016;73[9]:1089-98 ).
The EXPAND study was funded by Novartis. The lead author Dr. Kappos has received research and educational support funding via his institution from Novartis and multiple other pharmaceutical companies. Editorial author Dr. Metz has received grants from Roche and Biogen and personal fees from EMD Serono. The other editorial author, Dr. Liu, reported receiving personal fees from Novartis and personal fees and grants from EMD Serono. Dr. Liu was a back-up treating neurologist in the EXPAND trial.
SOURCE: Kappos L et al. Lancet. 2018 Mar 22. doi: 10.1016/S0140-6736(18)30475-6, and Metz L and Liu W. Lancet. 2018 Mar 22. doi: 10.1016/S0140-6736(18)30426-4 .