FROM CHEST
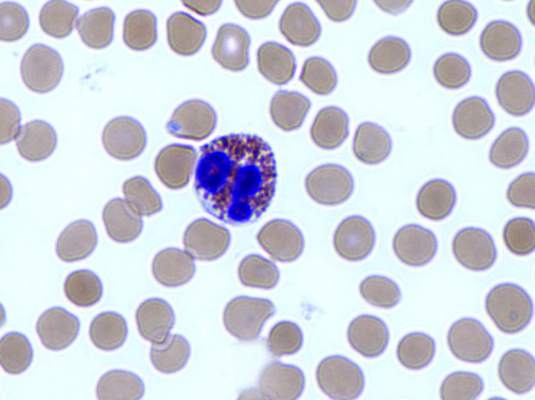
Reslizumab was most effective in patients with high baseline eosinophil counts, two randomized, placebo-controlled studies have determined. The companion studies were simultaneously published in the October issue of Chest.
The drug reslizumab, an anti–interleukin-5 monoclonal antibody, is made by Teva Branded Pharmaceutical Products R&D, who sponsored both studies.
The larger study, comprising 492 patients, found no significant benefit of reslizumab over placebo, Jonathan Corren, MD, and his colleagues wrote ( Chest. 2016;150:799-810 ). But this study didn’t stratify patients by baseline eosinophil levels; a post-hoc subanalysis found a significant benefit in forced expiratory volume in 69 of the patients who had at least 400 eosinophils/microliter (mcL) when treatment began.
The second study, which specifically targeted patients with a baseline eosinophil level of at least 400 cells/mcL, bolsters the conclusion that the drug works best in that population, said Leif Bjermer, MD, of Skane University, Lund, Sweden ( Chest. 2016;150:789-98 ).
In these patients, the drug significantly improved not only lung function, but asthma symptoms and asthma-related quality of life scores.
“These efficacy findings are consistent with results from other reslizumab trials and combined with the favorable safety profile observed, support the use of reslizumab in patients with asthma and elevated blood eosinophils, uncontrolled by an inhaled corticosteroid-based regimen,” Dr. Bjermer and his coauthors wrote.
The unstratified trial was conducted at 66 sites in the U.S. All of the patients had poorly controlled asthma despite using at least a medium-dosed inhaled corticosteroid. They were randomized to weekly infusions of reslizumab 3.0 mg/kg or placebo for 16 weeks.
The primary endpoint was the change in forced expiratory volume in one second (FEV1); secondary endpoints included quality of life scores; the need for rescue medication; forced vital capacity; and eosinophil count.
Patients in the placebo and reslizumab groups were an average age of 45.1 years and 44.9 years, respectively. The mean disease duration of patients in both groups was 26 years.
At week 16, the mean change in FEV1 from baseline was 255 ml in the active group and 187 ml in the placebo group – not a significant difference.
The team performed a post-hoc subgroup analysis that dichotomized the cohort based on baseline eosinophil levels. For the 343 with counts of less than 400 cells/mcL, there was no difference in FEV1 at 16 weeks, between the patients who received treatment and the patients who received a placebo. The FEV1s of these two groups were separated by just 33 mL.
The story was different for the 82 patients with at least 400 cells/mcL, with 69 of such patients receiving the drug and 13 of such patients receiving the placebo. At 16 weeks, the difference in FEV1 change was 270 mL, in favor of the active group. The strength of these findings may be weakened by the large difference in size between the treatment and placebo groups and the “near complete lack of response in the small number of placebo-treated patients.”
“Interpretation of the results in the [400 or more cells/mcL] subgroup is limited as the study was not designed or statistically powered to specifically test this group of patients,” the team wrote. Nevertheless, they concluded that reslizumab is a reasonable treatment option for this group. “These findings support an acceptable benefit-risk profile for reslizumab in asthma patients with a blood eosinophil threshold” of at least 400 cells/mcL.
The stratified study examined more endpoints: pre-bronchodilator spirometry (forced expiratory volume in one second FEV1, forced vital capacity, and forced expiratory flow), asthma symptoms, quality of life, rescue inhaler use, and blood eosinophil levels.
The 315 patients in this study all had a baseline eosinophil count of at least 400 cells/mcL. They were randomized to placebo or to 0.3 or 3.0 mg/kg reslizumab dose once every 4 weeks for 16 weeks. The mean ages for the patients taking the placebo, reslizumab 0.3 mg/kg, and reslizumab 3.0 mg/kg were 44.2, 44.5, and 43.0, respectively. The range of average disease durations for patients in the placebo group and two reslizumab groups was 20 to 20.7 years.
The final FEV1 was significantly improved over placebo in both active groups, although the change was much more pronounced in those taking 3.0 mg/kg, compared with those taking 0.3 mg/kg (160 mL and 115 mL, respectively, relative to placebo). Forced vital capacity also improved significantly in the 3.0 mg/kg dose group (130 mL relative to placebo).
Reslizumab was generally well tolerated in both studies. The most frequent adverse events in the stratified study were asthma worsening, headache, nasopharyngitis, upper respiratory infections, and sinusitis.
In the unstratified study, there were two anaphylactic reactions, but only one was related to the study drug. No deaths occurred in either treatment group of this study.
Both trials were sponsored by Teva. Dr. Bjermer has served on advisory boards or provided lectures for Aerocrine, Airsonett, ALK, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Meda, Mundipharma, Nigaard, Novartis, Regeneron, Sanofi-Aventis, Takeda, and Teva. Dr. Corren has been involved in speaker bureau activities for Genentech and Merck; he has served on advisory boards for Genentech, Merck, Novartis, and Vectura.
On Twitter @Alz_Gal