FROM THE JOURNAL OF VIRAL HEPATITIS
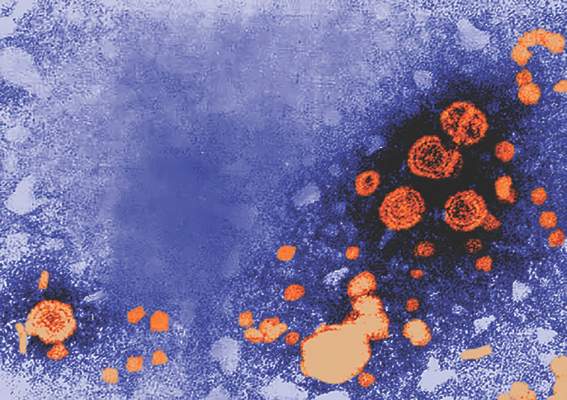
Patients coinfected with hepatitis B virus and HIV are at greater risk for in-hospital mortality, particularly in liver-related admissions, compared with HBV monoinfection, according to a study in the Journal of Viral Hepatitis.
Researchers at Massachusetts General Hospital, Boston, identified patients in the 2011 U.S. Nationwide Inpatient Sample who had been hospitalized with HBV or HIV monoinfection or HBV/HIV coinfection using ICD-9-CM codes. A total of 72,584 discharges with HBV monoinfection, 133,880 discharges with HIV monoinfection and 8,156 discharges with HBV/HIV coinfection were included. The researchers then compared liver-related hospital admissions among the three groups and performed multivariable logistic regression to identify independent predictors of in-hospital mortality, length of stay, and total charges.
According to Raymond T. Chung, MD , director of hepatology at Massachusetts General Hospital, and his coauthors, this study is the first to examine outcomes of HBV/HIV coinfection among hospitalized patients, a “group that represents those with advanced disease and vulnerable to poor outcomes and high health care utilization.” ( J Viral Hepat. 2016 Jun 13. doi: 10.1111/jvh.12555 )
Patients in the study with HBV monoinfection tended to be older than those with HIV monoinfection or HBV/HIV coinfection. Of those aged 51-65 years, 42% had HBV monoinfection, 34% had HIV monoinfection, and 31% had HBV/HIV coinfection (P less than .001). Males were overrepresented in the HBV/HIV coinfection group (77%), compared with those with HBV monoinfection (57%), and HIV monoinfection (67%). Additionally, the investigators found that patients with HBV monoinfection were more likely to be white (42%) than were those with HIV monoinfection (26%) or HBV/HIV coinfection (27%).
Dr. Chung and his colleagues found that HBV/HIV coinfection was associated with significantly higher adjusted in-hospital mortality, compared with patients with HBV monoinfection (adjusted odds ratio, 1.67; 95% confidence interval, 1.30-2.15), but not compared with HIV monoinfection (aOR, 1.22; 95% CI, 0.96-1.54).
“Interestingly, [the] increase in risk of mortality was primarily observed in liver-related admissions … and not infectious-related hospitalizations,” Dr. Chung and his coauthors said.
The overall adjusted hospital length of stay (LOS;1.53 days; 95% CI, 0.93-2.13; less than .001) and total hospitalization charges ($17,595; 95% CI 11,120-24,069; P less than .0001) were higher in the coinfected group, compared with the HBV monoinfection group – even after adjustment for comorbidity- and disease-related complications, the authors wrote. LOS and total charges also were higher in the coinfected group, compared with the HIV monoinfection group (+0.62 days; P = .034; $8,840; P = .005).
While HBV/HIV coinfection by itself was not associated with higher in-hospital mortality, the presence of HBV along with cirrhosis or complications of portal hypertension was associated with three times greater in-hospital mortality in patients with HIV, compared with those without such complications (odds ratio, 3.00; 95% CI, 1.80-5.02). Researchers also found that LOS (0.62 days; 95% CI, 0.05-1.20; P = .034) and hospitalization cost ($8,840; 95% CI, 2,604-15,077; P = .005) were increased in patients with HBV/HIV coinfection, compared with HIV monoinfection.
“Overall health care utilization from HBV/HIV coinfection is … higher than for either infection alone and higher than the national average for all hospitalizations, emphasizing the health care burden from these illnesses,” the authors concluded.
Three study coauthors were supported in part by grants from the National Institutes of Health, while one coauthor was supported by a career development award from the American Gastroenterological Association and by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Chung reported no financial conflict of interests. One coauthor reported participation on scientific advisory boards of AbbVie and Cubist pharmaceuticals.
On Twitter @richpizzi