Pharma brand managers deploy co-pay support programs for a host of reasons. Some of the most common of these include reducing patients’ concerns over out-of-pocket costs, overcoming managed care hurdles/timing, and supporting/expanding relationships with consumers and HCPs. But in many cases, behind all these reasons, lies a larger overarching goal: Increased patient adherence. In fact, the co-pay assistance industry initially sprang up as an effort to reduce Rx abandonment, which is a crucial first step in increasing adherence.
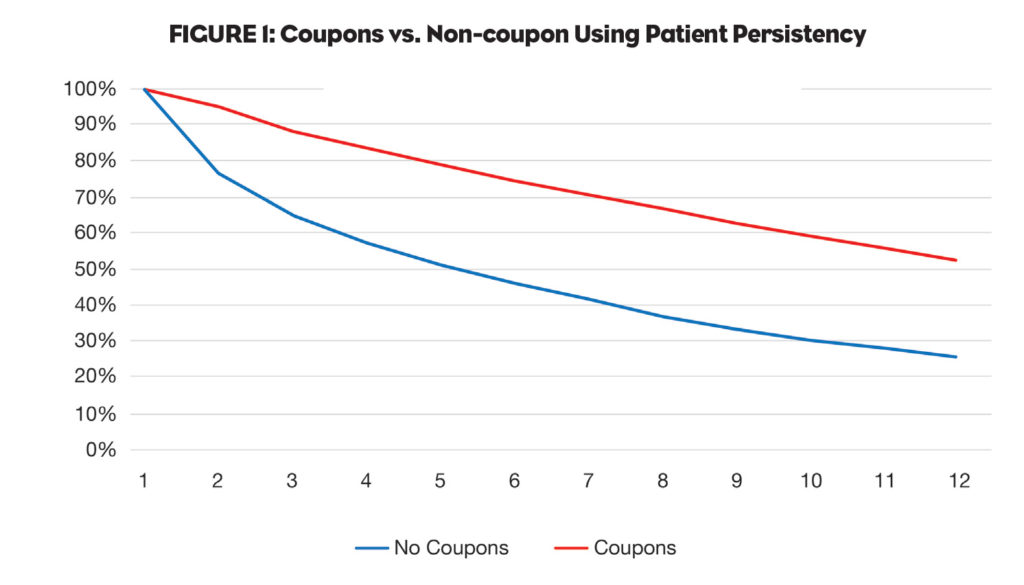
Ultimately, the use of co-pay assistance programs has expanded so rapidly over the past several years because they do indeed help get patients on therapy (primary adherence) and keep patients on therapy (secondary adherence). For example, Figure 1 (PSKW data) shows that coupon use across all channels for a representative CV drug is having a significant impact on patient adherence, with 52% of coupon users getting to their 12th fill versus only 25% for non-coupon users. (For more on this type of information, see the Wolters Kluwer data in an earlier article.1)
 What are the Proven Benefits of Increased Adherence?
What are the Proven Benefits of Increased Adherence?
But why do we fight so hard to increase adherence? Sure, if overall adherence increases to 60% from 50%, we see a sales increase (which is good for our company/brand and good for us). But beyond that, what’s so great about increased adherence? It seems intuitively obvious that better adherence should benefit patients, but has that ever been proven? And is there benefit elsewhere? Let’s take some time today to answer the question, “What are the proven benefits of increased adherence?”
Clinical Benefits of Increased Adherence
A large body of medical research has consistently shown that patients who take their medicine enjoy better health outcomes.2,3 After all, that is the point of controlled clinical trials: Taking Drug A yields a better clinical outcome than not taking Drug A. What’s more, patients who take their medicine spend less time in urgent care or in the hospital than those who don’t.4.5 If there were no clinical benefit to medication adherence, all of us should be (and would be) out of business.
Financial Benefits of Increased Adherence
It makes sense that since better adherence leads to better outcomes those better outcomes should translate into decreased healthcare utilization. And that has, in fact, been borne out in numerous studies. The real question for us is this: Does the decrease in overall healthcare service utilization, which occurs as a result of increased medication adherence, offset the increase in Rx spending that is also a result of increased adherence?
Marie Brown and colleagues discuss this exact issue in their April 2016 article, “Medication Adherence: Truth and Consequences.”6 They note an important study that examined the relationship between medication adherence in patients with chronic vascular conditions and the use and cost of healthcare services. As shown in Figure 2, increased adherence resulted in reduced total annual healthcare spending, with savings far beyond the relatively modest increase in Rx costs.
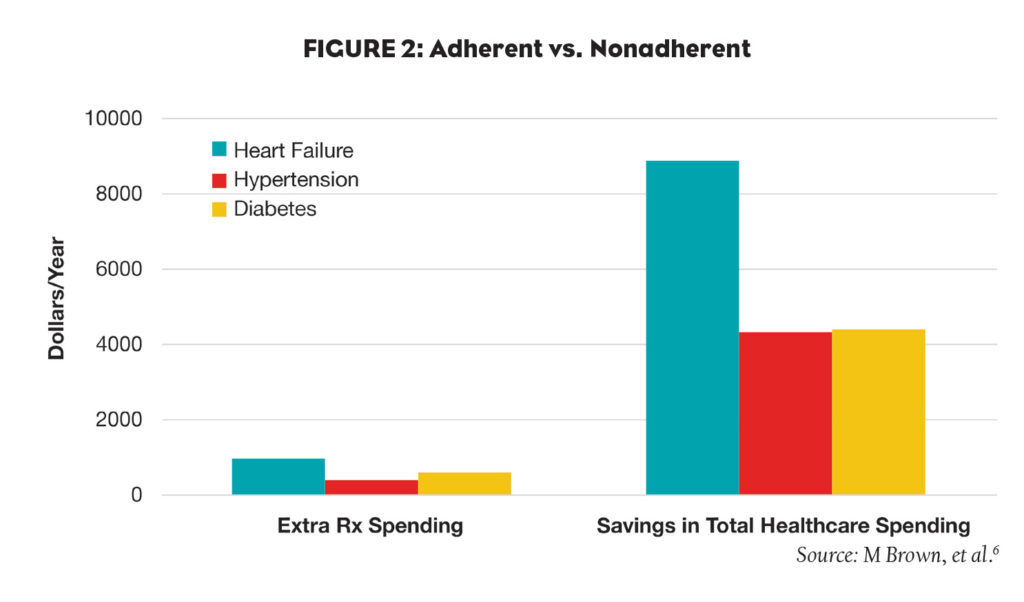 Extending this line of logic a bit further, Jha and colleagues estimated that improved adherence to diabetes medication alone could avert 699,000 emergency department (ED) visits and 341,000 hospitalizations annually, for a saving of $4.7 billion. 7
Extending this line of logic a bit further, Jha and colleagues estimated that improved adherence to diabetes medication alone could avert 699,000 emergency department (ED) visits and 341,000 hospitalizations annually, for a saving of $4.7 billion. 7
Connecting the Dots
If we lay these findings end to end, what do we see? Co-pay coupon use increases adherence, which improves clinical outcomes, which reduces ER visits and hospitalizations, which decreases infrastructure strain and saves payers (aka, “the system”) big money. And that’s why improving medication adherence is so important.
Three Simple Ways to Enhance the Connection Between Co-pay Programs and Increased Adherence
There’s no doubt that helping patients reduce their out-of-pocket cost is a vitally important part of the value delivered by co-pay programs. But here are some additional ways to augment programs to help them do an even better job of increasing adherence:
- Instead of allowing just three or six card uses, increase the number to 12. That one small change seems to increase patients’ perception of value, extending persistence.
- Instead of just offering a co-pay offset, build long-term relationships by layering on opt-in technology-enabled rapport builders like email and text messaging.
- Partner with a company that maintains a large EMR/EHR network—PDR, for example—and push alerts to HCPs regarding patient refills (or missed refills).
In the end, it’s good to know that doing well for ourselves can be positively aligned with doing good for patients and for “the system.” And it’s great to know that’s the case with using co-pay support to offset patients’ out-of-pocket costs.
References:
1. Dowd C. “Five Imperatives for Coupon and Co-pay Program Success.” PM360. Published online Aug 17, 2014. http://bit.ly/25Ivpb2.
2. DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. “Patient Adherence and Medical Treatment Outcomes: A Meta-analysis.” Med Care. 2002; 40(9):794–811.
3. McDermott MM, Schmitt B, Wallner E. “Impact of Medication Nonadherence on Coronary Heart Disease Outcomes: A Critical Review.” Arch Intern Med. 1997;157(17):1921–9.
4. Lau DT, Nau DP. “Oral Antihyperglycemic Medication Nonadherence and Subsequent Hospitalization Among Individuals with Type 2 Diabetes.” Diabetes Care. 2004;27(9):2149–53.
5. Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. “Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost.” Med Care. 2005;43(6):521–30.
6. Brown M, et al. “Medication Adherence: Truth and Consequences.” Am J Med Sci. 2016;351(4):387–399.
7. Jha AK, Aubert RE, Yao J, et al. “Greater Adherence to Diabetes Drugs is Linked to Less Hospital Use and Could Save Nearly $5 Billion Annually.” Health Aff (Millwood) 2012;31(8):1836–46.



