In the past decade, advances in technology and progress in drug innovation have led to many new and proven-effective strategies in disease prevention. Concurrently, healthcare systems have worked to expand their focus to bring more of these options to individuals and families, including vaccination programs, services encouraging physical activity, and technologies such as genetic testing that support early disease detection. Substantial research demonstrates that preventive care is often more efficient and cost effective than treatment of preventable diseases and their associated risk factors. These strategies have been shown to result in better health outcomes for patients and reduced burden on their families and caregivers.
As these advances in research and product development move forward, misalignment on what are considered adequate or optimal levels of preventive care among payers can create challenges for healthcare systems. This is especially evident in cases where preventive care involves a direct cost to payers and/or a significant time investment to patients, which can limit adoption or reimbursement. Our Life Sciences Practice team at CRA recently conducted an analysis to better understand the barriers to reimbursement for preventive care, how payer views might shift over the next decade, and how drug and technology companies focusing on preventive programs can optimize their strategies as the sector evolves.
Why are Payers Hesitant to Reimburse Preventive Measures?
Preventive care can deliver both clinical and economic benefits over the long term, but the business structure of many payers positions them to prioritize strategies that deliver short-term cost savings when making reimbursement decisions. They also recognize the significant upfront investment required to adopt and implement many preventive care services, which generally target large patient populations. Even if the cost per patient will be relatively inexpensive, many payers will see adoption of preventive measures as sub-optimal from a purely short-term economic standpoint.
The fact that payers have limited annual budgets can also lead them to deprioritize measures that require significant upfront costs but will not deliver a return on investment for several months or even years. The pressure to focus on short-term cost benefits may be even more pronounced in multi-payer systems where patients often move across payers. Many payers might consider that the economic benefits from an investment in preventive care will likely be accrued by a different payer as patients transfer.
Challenges in forecasting costs and patient demand can also make it difficult for payers to assess the true budget impact and cost effectiveness of preventive care measures. In one example, payers found that forecasting models used to predict the number of referrals received for the “Healthier You: NHS Diabetes Prevention Programme” in England, aimed to prevent or delay onset of type 2 diabetes, were inaccurate. After the program launched there were 16% more program referrals than initial estimates.1 While this revealed that the program was beneficial to a larger patient base, it also implies that the budget impact was underestimated, requiring NHS England to allocate more funding than initially forecasted.
Despite any uncertainties or challenges, some payers choose to invest in preventive care programs that offer longer-term societal and economic benefits. But research shows that among these payers many may not be allocating their funds as effectively as possible. On average, nearly 50% of all preventive care spending is allocated to patient monitoring (e.g., routine health or dental check-ups) rather than more effective methods such as immunization programs or technologies that support early disease detection.2
If preventive measures that can deliver cost benefits and improved health over the longer term are not implemented either at all or at target levels, healthcare systems risk a continued escalation in demand for care which, in turn, can be more costly than implementation of preventive measures in a timely manner.3
How Could Payer Views Change in the Years Ahead?
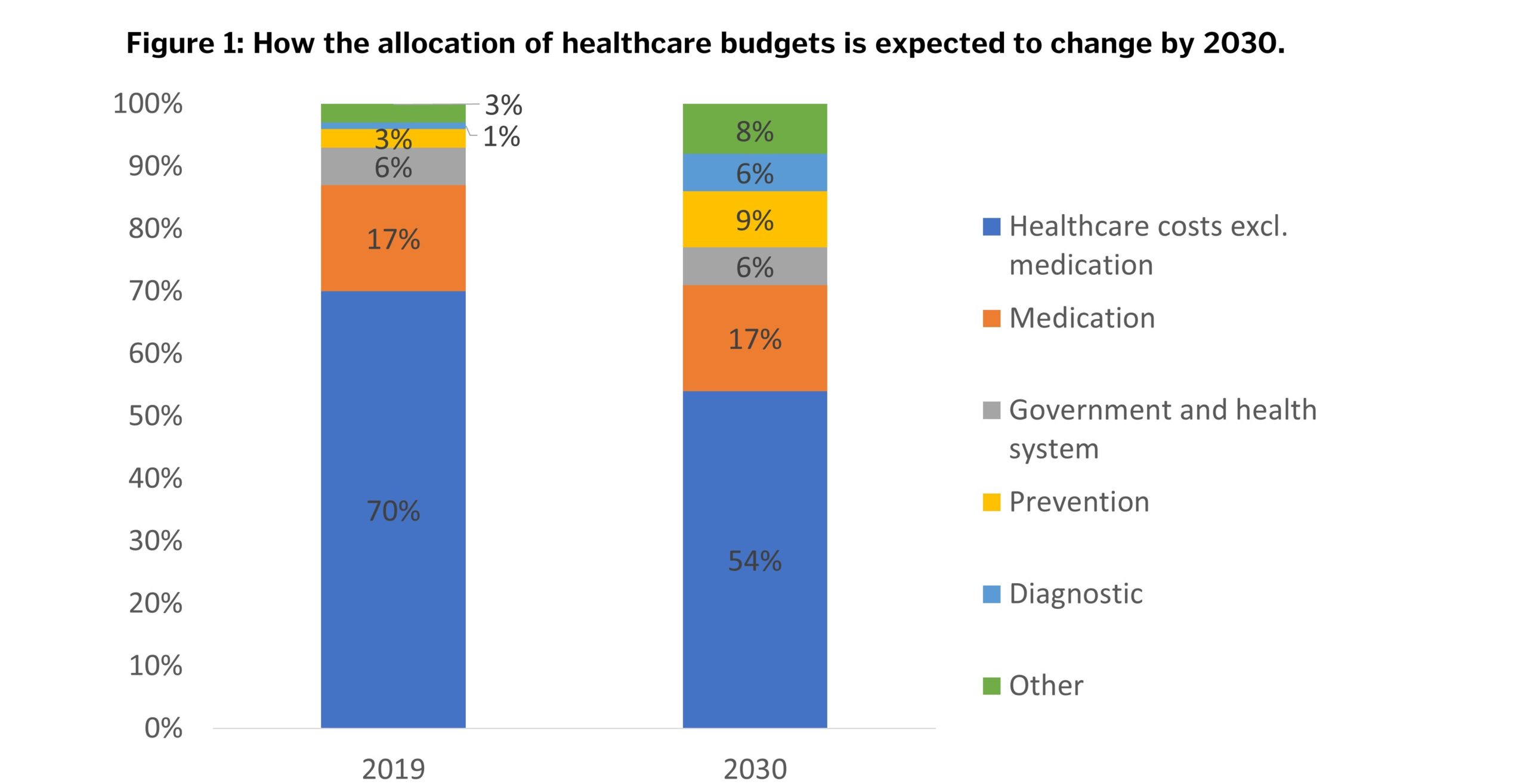
Currently, 3% of global healthcare budgets is allocated to preventive care—this number is expected to increase to 9% by 2030.4 In the years ahead more quantifiable data will likely be available demonstrating the longer-term benefits of preventive care, suggesting that payers may have fewer concerns over cost effectiveness. Some payers may also come under increased societal and governmental pressure to allocate more funding to preventive care services. For example, government advisors are proposing that Nordic countries should allocate equal amounts to sick care and preventive care (5% of GDP to each) by 2030.5
The fact that more targeted and effective treatments including potentially curative therapies are emerging in global markets could also position preventive care as a more cost-effective option, supporting the proposed shift in fund allocation. Investment in preventive measures could be considered more attractive to payers especially in cases where prevention can target higher risk populations.
Payers may also better recognize the value of preventive care over time as services become more targeted. With the increased availability of new technologies including wearable devices, health apps, and genetic testing, preventive care is rapidly improving. In one example, genetic testing would allow patients with a high risk of developing some diseases to receive more targeted preventive care, including routine screening and biomarker checks. This is currently the case for women with a variant of the breast cancer (BRCA) gene, which greatly increases their chance of developing breast and ovarian cancers and is readily identifiable through testing.6
How the Uptake of Preventive Measures May Evolve
Payer views aside, most industry stakeholders including leading medical organizations, government agencies, and life sciences companies consider preventive care to be a good investment. They understand that healthcare prevention practices can be critical for improving the general health of a population and are an essential component in addressing many major global health issues effectively. By 2030, healthcare professionals and medical organizations are expected to adopt more preventive care measures and promote them more effectively through educational and awareness campaigns.7
With an increasing range of more targeted and effective preventive care solutions available and in development, increasing willingness to pay for them—and growing demand by patients—the role and uptake of preventive care is expected to expand significantly by 2030. Companies developing preventive care services and programs will need to work to build broader awareness of their solutions among stakeholders including payers and patients. They will also need to provide education and training for healthcare professionals so they can accurately explain preventive care options to patients and perform services such as genetic testing.
It will be essential that companies play a role in improving coordination of preventive services between healthcare systems on local and global levels moving forward.8 By building optimal support and awareness of preventive care solutions, companies could help stakeholders to address recent issues in misallocation or limited allocation of budgets towards preventive care.
References:
1. Barron, E., Clark, R., Hewings, R., Smith, J. and Valabhji, J., 2018. “Progress of the Healthier You: NHS Diabetes Prevention Programme: Referrals, Uptake and Participant Characteristics.” Diabetic Medicine, 35(4), pp. 513-518.
2. OECD (2017), “How Much Do OECD Countries Spend on Prevention?”, available at [https://www.snop.it/attachments/article/775/OECD%20%20spese%20prevenzione.pdf].
3. WHO (2014), “The Case for Investing in Public Health”, available at [http://www.euro.who.int/__data/assets/pdf_file/0009/278073/Case-Investing-Public-Health.pdf?ua=1].
4. Strategy& (2019), “Driving the Future of Health – How Biopharma Can Defend and Grow its Business in an Era of Digitally Enabled Healthcare,” available at [https://www.strategyand.pwc.com/de/de/studien/2019/die-zukunft-der-gesundheit-vorantreiben/Driving-the-future-of-health.pdf].
5. Copenhagen Institute for Future Studies, “Nordic Health 2030”, available at [https://www.nordicinnovation.org/sites/default/files/2019/Nordic%20Health%202030%20Magazine.pdf].
6. NHS (2018), “Predictive Genetic Tests for Cancer Risk Genes,” available at [https://www.nhs.uk/conditions/predictive-genetic-tests-cancer/].
7. European Commission (2011), “Eurobarometer Qualitative Studies – Well-being in 2030”, available at [https://ec.europa.eu/commfrontoffice/publicopinion/archives/quali/wellbeing_aggregate_en.pdf].
8. Copenhagen Institute for Future Studies, “Nordic Health 2030”, available at [https://www.nordicinnovation.org/sites/default/files/2019/Nordic%20Health%202030%20Magazine.pdf].
Views expressed herein are the authors’ and not those of CRA or any of the organizations with which the authors are affiliated. The authors wish to acknowledge the contributions of Lev Gerlovin and Neil Turner to this article.









