PM360 asked those with the know-how to improve the patient experience what the industry can do to better serve patients during and following the global pandemic. Specifically, we asked them:
- COVID-19 is impacting how patients see their doctor, get medications, receive information, and much more. How else will the patient experience change because of the pandemic? And what can pharma companies offer patients to help improve this revamped healthcare experience?
- As patients desire to have more of a say in their treatments and the services being provided to them, how can life sciences companies make patients more of a partner in the development process? What are the keys to forming a successful, lasting, and trusting partnership?
 In the post-COVID world, continuing telehealth sessions as an alternative for office visits is a definite need. While virtual visits may be decreasing new medication starts for some, they’ve also led to patients focusing on taking their current medications as prescribed.
In the post-COVID world, continuing telehealth sessions as an alternative for office visits is a definite need. While virtual visits may be decreasing new medication starts for some, they’ve also led to patients focusing on taking their current medications as prescribed.
For example, we’ve seen late adopters of technology now enthusiastically tracking their symptoms—and HCPs encouraging that data collection to help monitor health status. Patients focusing on adherent behaviors, whether conscious or subconscious, is a positive outcome of the pandemic for both the patients and the HCPs managing their treatment.
At GSK, we’ve embraced the power of virtual engagement by expanding our Nurse Ambassador patient support program. We are activating and leveraging first-party data to better support patients at key points in time. Prior to COVID-19, we identified the need to shift patient engagement to a more personalized approach, and we are currently testing those experiences to understand their effectiveness.
As we look toward the future, armed with the knowledge of how COVID-19 is reshaping our environment, we’ll continue to use these learnings to provide a more dynamic engagement experience with an emphasis on nurse and telehealth support.
 The pandemic is creating a need for immediate gratification related to our health and wellness in three key ways.
The pandemic is creating a need for immediate gratification related to our health and wellness in three key ways.
1. HCPs “on call:” We’re all shifting from in-person to virtual and HCPs are not immune. HIPAA-compliant tools must be created to support this, much like Doximity’s app that enables HCPs to call patients anonymously on their own cell phones.
2. Alternative sites of care: The challenges of visiting one’s doctor is accelerating the opportunity for retail care sites such as CVS’s Health Hubs and Walmart Health. Pharma must incorporate these alternate sites into their marketing by targeting different types of providers (pharmacists, NPs/PAs) and optimizing materials for these locales (e.g., mobile geofencing vs. waiting room brochures).
3. Bite-sized health lessons: With health front and center there is a renewed focus on educating patients. However, this requires a shift—rather than large DTC campaigns, we must take a content marketing approach focused in digital and social channels. This will challenge pharma because today’s legal and regulatory process is not built to support this type of nimble work. Additionally, this content may not always be directly related to the brand, nor should it if we want patients to embrace it and follow us on social channels.
 It’s no surprise that patient engagement is going to increasingly take place virtually. Much of the conversation up until now has been about introducing patients to new technology that will connect them with their HCP. Moving forward, the conversation must shift to helping them learn to leverage these technologies to get the most out of them, as well as creating programs that make accessing a therapy easier.
It’s no surprise that patient engagement is going to increasingly take place virtually. Much of the conversation up until now has been about introducing patients to new technology that will connect them with their HCP. Moving forward, the conversation must shift to helping them learn to leverage these technologies to get the most out of them, as well as creating programs that make accessing a therapy easier.
In some cases, brands have the opportunity to connect them directly with a brand-educated HCP via telemedicine for a diagnosis and appropriate treatment. In other cases, brands can help empower patients with the information they need to educate their chosen HCP. Developing condition-specific tool kits designed to better prepare patients for what information the doctor will need is a way to make a virtual visit more productive for everyone involved.
In addition, you are going to see companies beginning to offer more resources by way of step-by-step instructions, including videos, on their websites for how patients can perform more at-home tests in conjunction with their doctor to determine optimal care. These changes to the patient experience bring more opportunity for patient empowerment and offer patients more control over their own health journey.
 Social media, more robust patient support programs, increased caregiver engagement, and a tsunami of online information have opened the door for everyone to have a seat at their own “health and wellness” table. Even conditions in which the physician has historically driven the treatment decision have seen a shift to a more collaborative approach. So how can life sciences companies ensure they embrace this dynamic and recognize the patient’s desire to be a part of the conversation?
Social media, more robust patient support programs, increased caregiver engagement, and a tsunami of online information have opened the door for everyone to have a seat at their own “health and wellness” table. Even conditions in which the physician has historically driven the treatment decision have seen a shift to a more collaborative approach. So how can life sciences companies ensure they embrace this dynamic and recognize the patient’s desire to be a part of the conversation?
Like most relationships, building a trusting, lasting partnership requires good communication. Frustration mounds when patients don’t feel heard or understood. Integrating simple feedback loops into patient communications via text, social media, and website content allows patients to tell you how they’re doing and what would make their experience better. Hosting a virtual co-creation lab with a group of patients enables real-time input on a specific initiative. Conducting surveys and focus groups gives patients the opportunity to share thoughts directly with you. Patients and caregivers will tell you what they want and need—it is up to you to listen.
 Even though the industry is placing a growing emphasis on partnering with patients in the development process, few are successful in doing so. Key considerations to pull it off:
Even though the industry is placing a growing emphasis on partnering with patients in the development process, few are successful in doing so. Key considerations to pull it off:
- Build patient engagement activities into the development plan and timeline.
- Create strategic relationships with patients through patient advocacy groups, physicians, or patient communities to facilitate ongoing dialogue.
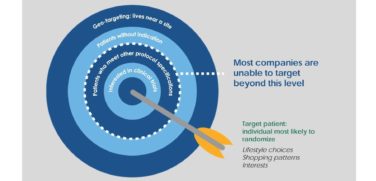
- Barriers, biases, perceptions, and concerns will vary across race, ethnicity, geographies, socio-economic levels, and cultures. Reaching more diverse patient populations requires a tailored and intentional approach to build trust, support, and increased interest in clinical trial participation.
- Endeavor to understand disease burden, patient preferences, barriers to healthcare and/or clinical trial participation, patient experiences, and risk tolerance.
- Consult experts in patient-centered research to build patient questionnaires, conduct patient panels, and build/validate instruments to ensure robust data collection and evidence of value.
- Incorporate embedded and exit interviews to evaluate the patient experience at key timepoints.
- Leverage patient input to modify design elements of the trial to ensure patients see value in the study objective, as well as to develop key messages to enhance enrollment.
- Provide patients with plain language summaries to recognize their contribution to the study, as well as a “thank you” for their study participation.
 Increasingly, patients want to engage in a dialogue and discuss the pros and cons of available options to get comfortable with the ultimate treatment decision. A critical piece of these conversations is the availability of quality patient educational material provided at the point of care. Through these materials, life sciences companies can help facilitate the dialogue and play an important role in this new, more patient-driven treatment decision process. However, in order to build trust and engage patients, it is critical these educational materials speak directly to patient concerns and convey a deep understanding of the patient experience.
Increasingly, patients want to engage in a dialogue and discuss the pros and cons of available options to get comfortable with the ultimate treatment decision. A critical piece of these conversations is the availability of quality patient educational material provided at the point of care. Through these materials, life sciences companies can help facilitate the dialogue and play an important role in this new, more patient-driven treatment decision process. However, in order to build trust and engage patients, it is critical these educational materials speak directly to patient concerns and convey a deep understanding of the patient experience.
Patient questions and concerns should be explicitly addressed in educational literature. To gain an accurate understanding of these concerns, companies should focus on the patient journey and the questions they are asking physicians during clinical visits.
Additionally, companies must understand the non-clinical factors that influence patient preferences. Concerns around the impact on quality of life and on unique lifestyle circumstances are now playing a greater role in treatment decisions. By acknowledging the patient’s viewpoint in educational materials, companies can demonstrate that they value the patients as individuals and want to provide them with a positive experience.