AT ID WEEK 2017
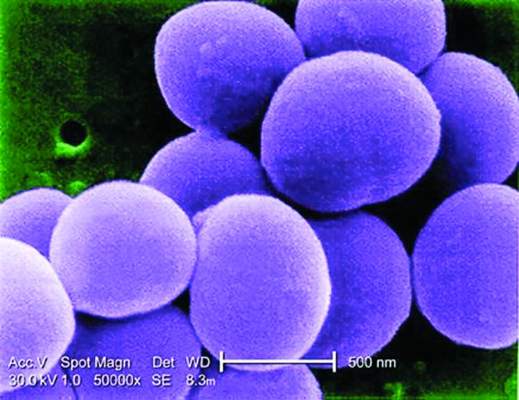
SAN DIEGO (FRONTLINE MEDICAL NEWS) – By standardizing antibiotic treatment for simple and uncomplicated staphylococcal bloodstream infections (BSI), an algorithm effectively shortens therapy and simplifies decision making, according to results of a multinational randomized trial.
“The data from the study confirm that the algorithm achieves more with less and verify that shorter antibiotic courses are sufficient,” reported Thomas L. Holland, MD , an infectious disease specialist at Duke University Hospital in Durham, N.C.
Several cases of complicated staphylococcal BSI found their way into the study despite selection criteria designed to enroll only uncomplicated cases. This was inevitable because not all cases destined to become complicated can be identified initially, but outcomes overall still remained similar between the algorithm and standard of care (SOC) groups.
In this study, the patients randomized to algorithm treatment received vancomycin (or daptomycin in allergic or intolerant patients), which was administered for periods of duration based on clinical features. In those randomized to SOC, the choice and duration of antibiotics were left to the discretion of the treating physician without restrictions.
In those with simple staphylococcal BSI, the algorithm called for no further antibiotics beyond what had already been administered empirically prior to randomization. Key features of simple coagulase-negative staphylococcal (CONS) BSIs include absence of fever or evidence of metastatic infection, as well as no more than one positive follow-up blood culture. The key features of simple Staphylococcus aureus BSI are similar. However, no positive blood cultures are required for S. aureus BSI to be classified as simple.
“In the algorithm arm, no antibiotics were given to those with simple staphylococcal BSI unless antibiotics had been given prior to randomization,” Dr. Holland explained, but he acknowledged that empiric antibiotics prior to randomization reflect “clinical reality.”
In those with uncomplicated rather than simple staphylococcal BSI, vancomycin was given for 5 days to those with CONS BSI and for 14 days to those with S. aureus BSI. In those who were randomized and then subsequently found to have a complicated infection, defined as multiple positive blood cultures or evidence of metastatic infection, patients received as few as 7 days or as many as 28 days of antibiotics, “reflecting the heterogeneity of these infections,” Dr. Holland reported at an annual scientific meeting on infectious diseases.
The coprimary endpoints were treatment success at test of cure and treatment safety, both of which were adjudicated by an external committee consisting of infectious disease specialists blinded to the therapy.
There were 509 patients from 16 sites in both the United States and Spain. CONS BSIs represented approximately 75% of patients in both arms. The complicated staphylococcal infections, which also were evenly distributed in the two arms, were included in the intention-to-treat analysis. Of complicated staphylococcal infections in this study, the pathogen was CONS in 34 instances and S. aureus in 37.
Treatment success was achieved in 82.0% and 81.5% of patients in the algorithm and SOC arms, respectively. Significant adverse events occurred in 32.9% and 28.3% of patients, respectively. Neither difference approached statistical significance.
“In other words, the algorithm was as effective and safe as standard of care,” Dr. Holland confirmed.
However, the median duration of treatment was reduced substantially for those randomized to the algorithm arm, compared with that seen in the standard of care arm. Among evaluable patients without complicated BSI, the mean duration of therapy was 4.4 days in the algorithm group vs. 6.2 days in the SOC group (P = .003). Most of this nearly 2-day reduction in treatment was achieved in uncomplicated CONS BSI patients. In this group, the mean days of treatment were 5.3 days and 8.4 days for the algorithm and SOC groups, respectively. In the uncomplicated S. aureus group, the reduction (from 15.9 to 15.3 days) was not significant.
“The study has several messages. For one, it suggests that patients who meet the criteria of simple staphylococcal BSI can be managed safely with monitoring alone. In addition, this study “provides the best evidence to date that 14 days of vancomycin from the first negative blood culture is sufficient in uncomplicated S. aureus bloodstream infections,” Dr. Holland stated.
“For many, these data will validate what they are already doing,” said Dr. Holland, who reported that the algorithm is now being applied routinely at his institution. “The value is that we now have a randomized trial to demonstrate that shorter therapy can be provided in uncomplicated staphylococcal blood stream infections without increasing risk of serious adverse events.”