The impact—and volume—of prior authorizations required for specialty prescriptions in the U.S. has increased in recent years in line with the increase in the percent, and total spend, for specialty pharmaceuticals overall.
Today, a typical physician office visit resulting in a prescription for the patient often “ends” at the pharmacy where the patient is asked to contribute their co-pay based on their insurance coverage as well as the formulary coverage. However, for a growing number of patients (and prescriptions) there is an added step in the process—the dreaded prior authorization (PA). For the individual patients confused by the process, it often adds hours—if not days—to the Rx fill process. For the physicians and their staff, it is a very frustrating and inefficient process that requires a constant stream of asynchronous back and forth communication with the payers (i.e., health plans and/or the pharmacy benefits manager [PBM]) to demonstrate clinical need and to satisfy the individual and ever changing PA guidelines.
Seeking to quantify the economic impact to the typical practice, one study conducted in 2012 and published in the Journal of the American Board of Family Medicine pegged the annual cost to a typical family practice at $2,161 to $3,430. Spending time on an administrative process that ultimately drives value for the patient is one thing. Spending time on a process that is intentionally designed to be archaic, timely, and often frustrating for both the patient and the practice is another. Physicians, patients, and the pharmaceutical industry must focus on promoting the use of digital to inject much needed efficiency into the PA process to drive value throughout the healthcare system.
The State of Prior Authorization
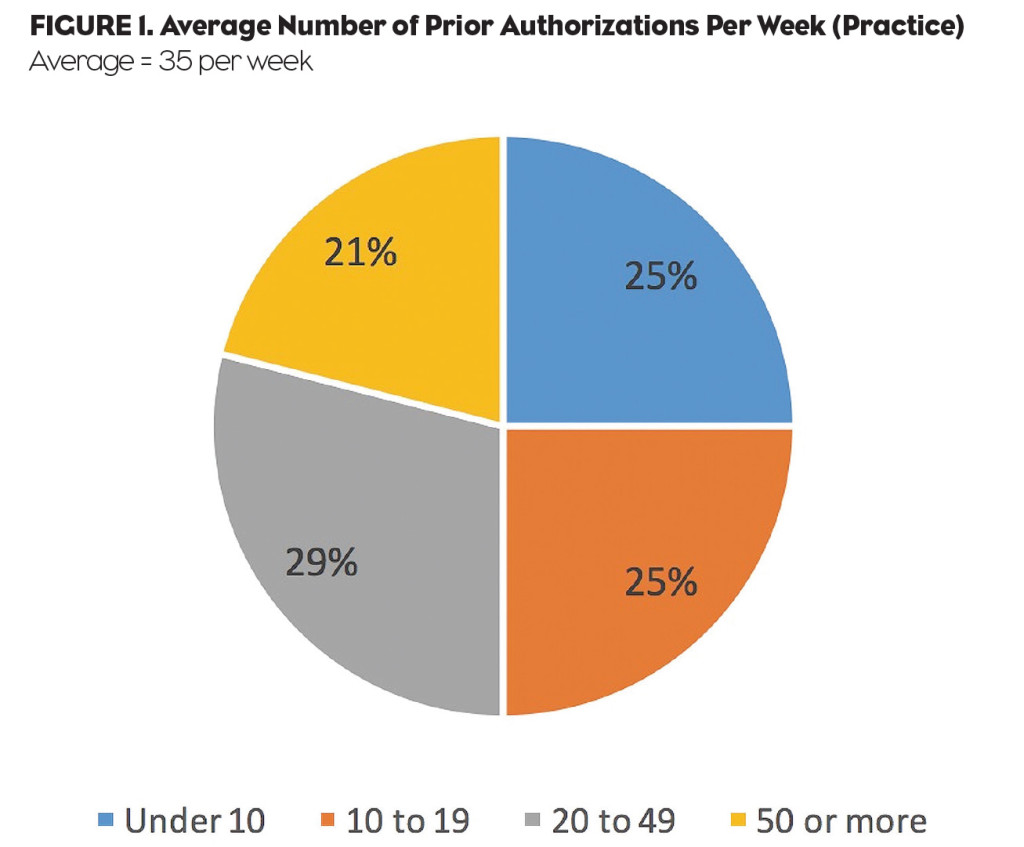
In an effort to better understand the state of prior authorization today and impact on their practice, jumpRx conducted a study in Q1 2016 with a group of 400 U.S. physicians (across multiple specialties). The average physician (for all specialties) completed 35 prior authorizations per week. Looking at differences between the specialty segments, rheumatologists tended to be more active with PA (at 44 per week on average) compared with primary care physicians averaging 31 per week.
The study also found that one in five U.S. physicians complete 50 or more PAs per week—and roughly a third complete 20 to 49 PAs per week (Figure 1). In other words, processing prior authorizations is not limited to a defined segment of physicians just dealing with the most expensive drugs. It is a widespread issue impacting a broad segment of physician prescribers and customers today.
 In addition to the pure volume and hassles of dealing with PA in the practice, knowing ahead of time whether or not a desired prescription product will require a PA presents a real challenge for the average physician, practice, and their staff. Sixty-three percent of all U.S. physicians report they are “not sure” if a desired prescription they are going to prescribe for a patient will require a prior authorization at the time they decide to prescribe the medication. The numbers jump to 71% for cardiologists. In other words, almost three in four U.S. cardiologists are not sure if the Rx they are writing will require a PA at the time they deem the treatment necessary for their patients.
In addition to the pure volume and hassles of dealing with PA in the practice, knowing ahead of time whether or not a desired prescription product will require a PA presents a real challenge for the average physician, practice, and their staff. Sixty-three percent of all U.S. physicians report they are “not sure” if a desired prescription they are going to prescribe for a patient will require a prior authorization at the time they decide to prescribe the medication. The numbers jump to 71% for cardiologists. In other words, almost three in four U.S. cardiologists are not sure if the Rx they are writing will require a PA at the time they deem the treatment necessary for their patients.
The Burden on the Practice
Knowing the volume of PA in the U.S. today is just the first step in understanding the real impact. According the research study by jumpRx, 59% of physicians in the U.S. report that prior authorization is an “immense” or “significant” burden to their practice today (Figure 2). In other words, for the majority of U.S. physicians (and their staff) the PA process is a major headache.
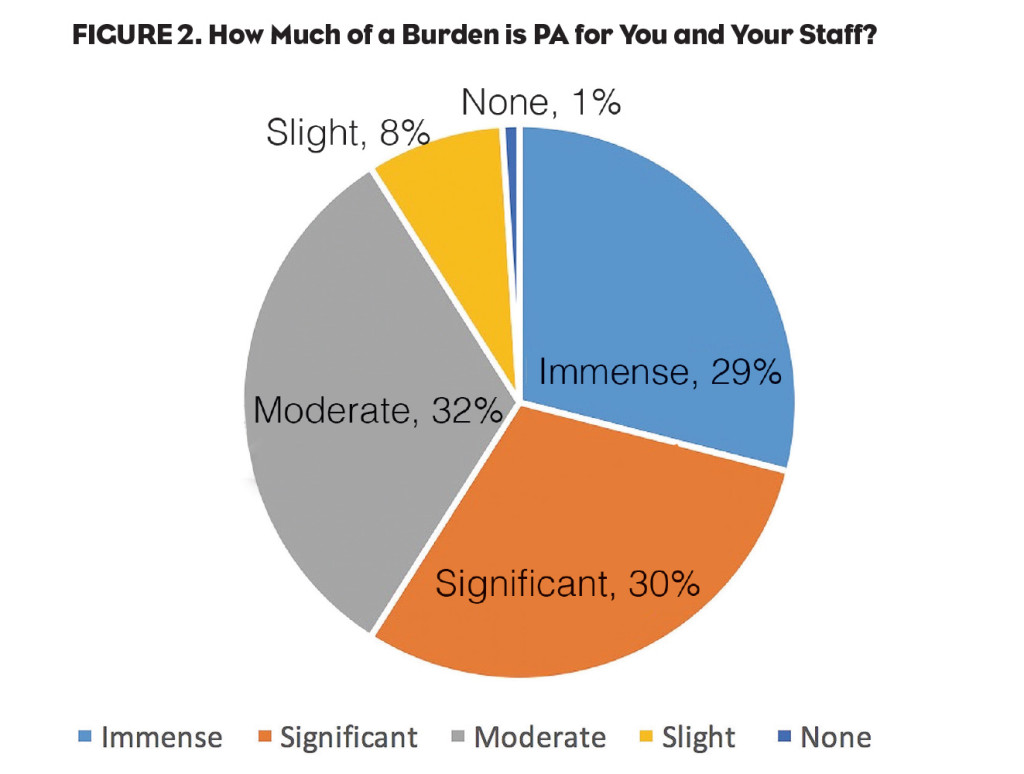 Similar to the differences in knowing whether an Rx will require PA (or not), there are also differences between specialty segments when looking at the burden of PA on the practice. For example, 75% of rheumatologists state that PA is an “immense” or “significant” burden on their practice. In other words, only one in four rheumatologist practices is not impacted by PA in a major way today.
Similar to the differences in knowing whether an Rx will require PA (or not), there are also differences between specialty segments when looking at the burden of PA on the practice. For example, 75% of rheumatologists state that PA is an “immense” or “significant” burden on their practice. In other words, only one in four rheumatologist practices is not impacted by PA in a major way today.
The results highlight a major opportunity for pharmaceutical brands seeking to add value at the practice level specific to a real “pain point” today for most physicians. Of course all this insight into the current state of PA generates a few questions: Are physicians interested in pharmaceutical-sponsored tools and resources specific to prior authorization (forms and guidelines)? If so, how would they want to access that information in their practice?
Using Digital Rx Resources
After drilling down into the impact of PA on the practice, the research study then reviewed a group of pharmaceutical information resources, as well as the format and method by which physicians would like to access the info (Figure 3). Eighty-four percent of U.S. physicians are interested in accessing PA forms online that are specific to the plans they accept and the drugs they prescribe (usually a customized short list).
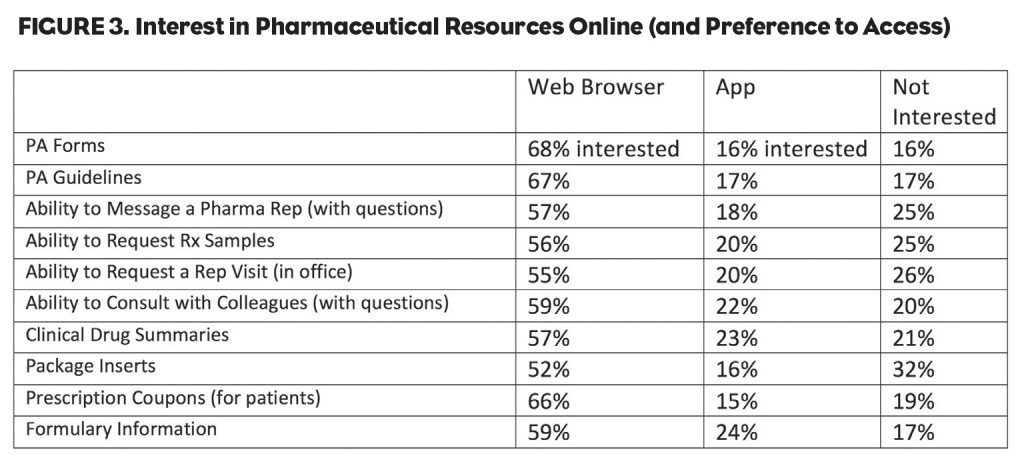 When looking at the desired format to access the PA information, 68% prefer to access through a Web browser (desktop or laptop) and only 16% preferred to access via an app on their phone. The numbers change slightly between specialty segments, but physicians in the U.S. overwhelmingly prefer to access the information through a Web browser for PA forms.
When looking at the desired format to access the PA information, 68% prefer to access through a Web browser (desktop or laptop) and only 16% preferred to access via an app on their phone. The numbers change slightly between specialty segments, but physicians in the U.S. overwhelmingly prefer to access the information through a Web browser for PA forms.
In addition to the PA forms online, 83% are interested in accessing the PA guidelines online (requirements for approval), 67% prefer to access through a Web browser and 17% prefer to access through an app. Again, the numbers were consistent when comparing across specialty segments—the vast majority prefer to access PA guidelines through a Web browser.
The jumpRx study also reviewed a number of different pharmaceutical-related resources online for context and comparison to online PA forms. PA forms and guidelines sit at the top of the wishlist of useful resources, further underlining the opportunity.
The Next Stage of PA?
Given the rapid movement to digitize clinical information in the practice, the current antiquated fax-based PA process is a major challenge—and source of frustration—for many physicians today. Meanwhile, the study also revealed only limited traction among physicians seeking to explore alternatives, such as electronic solutions to help inject efficiency into the PA process.
According to the jumpRx study, only 12% of U.S. physicians (across specialty segments) are currently using some type of software or online platform to process their prior authorizations. Among those using software or an online platform, 38% report the software or platform is currently integrated with their EMR system. In other words, the vast majority of physician practices today remain mired in the chaos of the current fax-based system, and among a small segment using software or an online platform, less than half are fully integrated with their EMR.
So what does this mean for the average physician practice—and for pharmaceutical brands they prescribe? As the number of specialty prescriptions continues to increase, the need for digital resources with updated, real-time and accurate PA information will continue to increase at the practice level. Furthermore, as existing digital PA platforms continue to integrate and align with the health plans and PBM side of the business, it will become increasingly important for pharmaceutical companies—and brands—to seek out alternative strategies if they choose to remain relevant and an integral part of the PA process. One approach could be to provide physician customers with the latest information about PA forms and guidelines in an effort to expedite the process and to remove the headaches (and exasperation) currently associated with the PA process.
While getting to a world where “PA does not exist” does not seem to be a likely option—despite the pleas of physicians—as a healthcare system we must do a much better job of providing physicians, their staff, pharmacists, and the patients with efficient and effective tools and resources. In addition to making sure physicians have the latest PA information, as a system we must also strive to reduce the “leakage” and the lost prescriptions as a result of the current broken PA system. Minimizing those abandoned prescriptions for desired innovative products is something that everyone can live with—physicians, patients, and even the payers.






