Interpreting new 2017 syncope guideline
EXPERT ANALYSIS FROM AAP 2017
CHICAGO (FRONTLINE MEDICAL NEWS) – Syncope often is misdiagnosed in pediatric patients complaining of chest pain, and a new guideline released in 2017 could guide clinicians toward a more accurate differential diagnosis and help them know when immediate referral to cardiology or the emergency department is warranted.
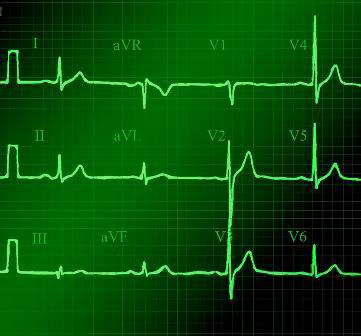
“There are recent guidelines published this year which are helpful,” said Dr. Barbara Deal, the Getz Professor of Cardiology at Northwestern University in Chicago. “I’d like you to pay attention to the fact that the [guideline states] that a 12-lead ECG should be performed in all pediatric patients presenting with syncope,” which is defined as transient loss of consciousness.
The ECG is indicated because “sometimes it’s hard to know if something was vasovagal or not. Even for me, I still sometimes get it wrong.” The 12-lead ECG is recommended for the first but not every episode, according to the 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. Although this guideline was developed by groups that typically focus more on adults, the Pediatric and Congenital Electrophysiology Society endorsed the guideline.
“Once you establish it is a simple vasovagal [cause], you need to educate patients on conditions that would promote this and the need to be anticipatory,” Dr. Deal said at the annual meeting of the American Academy of Pediatrics. “Further testing with an echo[cardiogram] should be done if you suspect heart disease or a rhythm disorder.”
Chest pain and syncope are common complaints that can lead to significant anxiety for patients, parents, and pediatric providers. The greatest cause of this anxiety is the prospect of a fatal or near-fatal event. An abnormal cardiac examination, any associated palpitations, and a history of urinary incontinence or traumatic injury are reasons to worry, she said. “Any of these should prompt an urgent consult to cardiology or the emergency department.”
Cardiac causes of chest pain include reflex or vasovagal syncope or even a more serious cardiac cause, such as arrhythmic or structural issues, Dr. Deal said. Symptoms that appear with exertion or stress also are very worrisome. “You would know if they have a heart murmur or stenosis – it’s these other things that don’t present with a cardiac abnormality: hypertrophic cardiomyopathy or arrhythmogenic right ventricular cardiomyopathy,” she said. “If they have symptoms on exertion, pay attention. This is not good.”
Syncope often is misdiagnosed, Dr. Deal said. Approximately 35%-48% of patients classified as having syncope do not have actual syncope. In a study of 194 children, for example, the leading etiologies diagnosed after evaluation for syncope included simple fainting in 49%, a vasopressor/vasovagal response in 14%, and possible seizure in 14% ( J Am Coll Cardiol. 1997;29[6]:1039-45 ). Only 7% were diagnosed with syncope in this series. Some other causes included psychogenic or orthostatic ones, hyperventilation, dysmenorrhea, vertigo, dehydration, trauma, stress, exhaustion, or an infectious condition.
“When should you be thinking life-threatening syncope?” Dr. Deal asked. Arrhythmic disorders that are heritable, such as an ion channelopathy, are an example. “They don’t always feel the racing heartbeat, but they feel something is not right; they feel a sense of impending doom. Some families report signs during exercise like swimming, seizures, gargling noises, or unusual symptoms on awakening.”
Dr. Deal noted that ages 3-24 years are “the problem territory for cardiac arrest.” In this age group, 43%-55% of chest pain–related episodes are associated with hypertrophic cardiomyopathy or arrhythmias; about one in three will have prior syncope. “These causes are not detectable on physical examination and often are not detectable with ECG only,” adding to the differential diagnosis challenges.
Refer to a pediatric cardiologist
For this reason and others, referral to a pediatric cardiologist is indicated instead of a consult with an adult cardiologist, Dr. Deal said. “You know how your kids will start with ‘no offense.’ Like, ‘no offense, Mom, but your hair looks awful.’ With moderate offense intended, having an adult cardiologist read a pediatric ECG and clear them is not adequate. They will be looking for ischemia or A-fib [atrial fibrillation]; they’re not looking for long QT syndrome, arrhythmogenic cardiomyopathy, or abnormal T waves.”
Early detection of long QT syndrome is optimal, Dr. Deal said, because symptom onset often is between infancy and age 7 years. In addition, mortality is highest in the first 2 decades of life. “I think this could be why adult cardiologists are not as concerned as we are,” Dr. Deal said. “The bad ones die before they reach adulthood.”
Ruling out a cardiac cause
The 2017 joint guideline defined syncope as a transient loss of consciousness. “By definition, you pass out, you’re not aware of where you are, and you cannot hear,” Dr. Deal said. If a patient reports they could hear people talking, they may have lost postural tone, but they did not have syncope, she added.
“Sometimes, we see teenagers who are said to pass out and are unresponsive for 5 minutes, 10 minutes, or 20 minutes. I’m usually relieved to hear that because that gets cardiac off the hook,” Dr. Deal said. “There is nothing cardiac that makes you pass out for 20 minutes, unless people are resuscitating you.” She added, “I’m not suggesting it’s not a significant problem that you need to get to the bottom of.”
Noncardiac etiologies can be neurologic, metabolic, drug-induced, or psychogenic. “This is where the detective work comes in.”
Keep clinical suspicion high for psychogenic syncope, Dr. Deal said. Psychogenic episodes stem from significant psychological stress, often something so profoundly bothersome that they cannot cope, such as sexual abuse.
A helpful tip for diagnosing the less worrisome vasovagal syncope is asking whether a patient was sitting to standing or standing a long time before an episode, Dr. Deal said. “A common complaint is that the family went to airport, got up early, didn’t eat, and ended up standing for a long time. Kids will say they don’t feel well, they fall down, and all hell breaks loose.” Other causes of vasovagal syncope include stress, pain, or a situational trigger, for example, when a person faints during a blood draw or immunization.
The 2017 guideline also set forth the evidence behind various medications used to lower the risk of syncope. However, Dr. Deal said, “If syncope only happens every 3 years when you go to an airport, it’s probably not worth daily therapy to prevent that.”
‘The world’s most boring test’
For the most part, lifestyle measures should work to address vasovagal syncope. A tilt table test can be useful to aid the differential diagnosis, but it’s recommended only when the etiology is unclear, Dr. Deal said. On the plus side, the tilt table test allows clinicians to reproduce symptoms in a controlled environment. On the downside, she added, “It’s the world’s most boring test. It’s a challenge for the cardiologist to stay awake. It’s very boring, until all hell breaks loose.”
“I find this helpful in the setting of kids with seizures and for kids with this atypical syncope where you just cannot convince the family that these 20-minute episodes of loss of consciousness are not near-death episodes.”
Dr. Deal had no relevant financial disclosures.