Question: Which of the following statements regarding Shinal v Toms, a recent landmark decision on informed consent, is correct?:
A. The case was heard in the Pennsylvania Supreme Court and its decision is binding only in that state.
B. It held that obtaining informed consent is a doctor’s duty that is non-delegable.
C. The decision reversed the lower courts, which had held that the defendant’s qualified assistant could obtain consent.
D. An earlier case heard by the same court had ruled that doctors, not hospitals, owe the legal duty to obtain informed consent.
E. All are correct.
Answer: E.
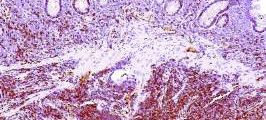
On November 26, 2007, Megan Shinal and Dr. Steven Toms met for a 20-minute initial consultation to discuss removing a recurrent craniopharyngioma.1 Years earlier, a surgeon had performed a transsphenoidal resection, but was unable to remove all of it. The residual portion of the tumor had increased in size and extended into vital structures of the brain, jeopardizing Mrs. Shinal’s eyesight and her carotid artery, causing headaches, and threatening to impact her pituitary function.
Dr. Toms testified that he reviewed with Mrs. Shinal the alternatives, risks, and benefits of total versus subtotal resection, and shared his opinion that, although a less aggressive approach to removing the tumor was safer in the short term, such an approach would increase the likelihood that the tumor would regrow. Dr. Toms was unable to recall many of the specifics, but he testified that he advised Mrs. Shinal that total surgical resection offered the highest chance for long-term survival. By the end of the visit, Mrs. Shinal had decided to undergo surgery. However, the type of surgery had not yet been determined.
Shortly thereafter, on December 19, 2007, Mrs. Shinal had a telephone conversation with Dr. Toms’ physician assistant. Mrs. Shinal later testified that she asked the physician assistant about scarring that would likely result from surgery, whether radiation would be necessary, and about the date of surgery. The medical record of this telephone call indicated that Dr. Toms’ physician assistant also answered questions about the craniotomy incision. On January 17, 2008, Mrs. Shinal met with the physician assistant at the Geisinger Medical Center’s Neurosurgery Clinic. The assistant obtained Mrs. Shinal’s medical history, conducted a physical, and provided Mrs. Shinal with information relating to the surgery. Mrs. Shinal signed an informed consent form.
On January 31, 2008, Mrs. Shinal underwent an open craniotomy for a total resection of the pituitary tumor at Geisinger Medical Center. During the operation, Dr. Toms perforated Mrs. Shinal’s carotid artery, which resulted in hemorrhage, stroke, brain injury, and partial blindness.
According to the Shinals’ complaint, Dr. Toms failed to explain the risks of surgery to Mrs. Shinal or to offer her the lower risk surgical alternative of subtotal resection of the benign tumor, followed by radiation. At trial, Mrs. Shinal was unable to recall being informed of the relative risks of the surgery, other than coma and death. She testified that, had she known the alternative approaches to surgery, i.e., total versus subtotal resection, she would have chosen subtotal resection as the safer, less aggressive alternative.
The trial court instructed the jury with regard to Dr. Toms’ duty to obtain informed consent from Mrs. Shinal as follows: “[I]n considering whether [Dr. Toms] provided consent to [Mrs. Shinal], you may consider any relevant information you find was communicated to [Mrs. Shinal] by any qualified person acting as an assistant to [Dr. Toms].”
On April 21, 2014, the jury returned a verdict in favor of Dr. Toms.
The plaintiffs appealed to the Pennsylvania Superior court, which affirmed the trial court’s judgment. It rejected the Shinals’ argument that the trial court’s informed consent charge, which permitted the jury to consider information provided by Dr. Toms’ physician assistant to Mrs. Shinal, was erroneous and prejudicial. The Superior Court relied upon two of its prior cases to opine that a qualified professional acting under the attending doctor’s supervision may convey information communicated to a patient for purposes of obtaining informed consent.
The trial court initially instructed the jury that, in assessing whether Dr. Toms obtained Mrs. Shinal’s informed consent, it could consider relevant information communicated by “any qualified person acting as an assistant” to Dr. Toms. The defendant doctor argued that while it is the physician’s duty to obtain the patient’s informed consent, the physician is not required to supply all of the information personally. It is the information conveyed, rather than the person conveying it that determines informed consent. Dr. Toms cited several older Pennsylvania Superior Court cases, which permitted a physician to fulfill through an intermediary the duty to provide sufficient information to obtain a patient’s informed consent.
The plaintiffs then appealed to the Pennsylvania Supreme Court, which led to a reversal. In a 4-3 decision, the Court disagreed, citing their ruling in the 2002 case of Valles,2 where they held that the duty to obtain informed consent could not be imputed to a hospital. In Valles, the Court held that the duty to obtain a patient’s informed consent is a non-delegable duty owed by the physician conducting the surgery or treatment, because obtaining informed consent results directly from the duty of disclosure, which lies solely with the physician, and a hospital therefore cannot be liable for a physician’s failure to obtain informed consent.
Reasoning by extension, the Court accordingly ruled that a physician may not delegate to others his or her obligation to provide sufficient information in order to obtain a patient’s informed consent. It declared: “Informed consent requires direct communication between physician and patient, and contemplates a back-and-forth, face-to-face exchange, which might include questions that the patient feels the physician must answer personally before the patient feels informed and becomes willing to consent. The duty to obtain the patient’s informed consent belongs solely to the physician.” The Court held that “a physician cannot rely upon a subordinate to disclose the information required to obtain informed consent. Without direct dialogue and a two-way exchange between the physician and patient, the physician cannot be confident that the patient comprehends the risks, benefits, likelihood of success, and alternatives… Informed consent is a product of the physician-patient relationship. The patient is in the vulnerable position of entrusting his or her care and well being to the physician based upon the physician’s education, training, and expertise. It is incumbent upon the physician to cultivate a relationship with the patient and to familiarize himself or herself with the patient’s understanding and expectations. Were the law to permit physicians to delegate the provision of critical information to staff, it would undermine patient autonomy and bodily integrity by depriving the patient of the opportunity to engage in a dialogue with his or her chosen health care provider. A regime that would countenance delegation of the informed consent process would undermine the primacy of the physician-patient relationship. Only by personally satisfying the duty of disclosure may the physician ensure that consent truly is informed.”
The facts of the case appear straightforward, and its legal conclusion clear. Whether one agrees with the Court’s decision is, however, another matter. The AMA and the Pennsylvania Medical Society (PAMED) had submitted an amicus brief supporting Dr. Toms’ position, arguing that he had fulfilled his obligations under Pennsylvania’s Medical Care Availability and Reduction of Error (MCARE) Act as well as common law established in previous Pennsylvania court rulings. The final appellate decision therefore came as a big disappointment. The PAMED website notes that the decision “could have significant ramifications for Pennsylvania physicians” in that they can “seemingly no longer rely on the aid of their qualified staff in the informed consent process.”3 The urgent question now is whether other jurisdictions will adopt this Pennsylvania rule that drastically changes the way doctors obtain informed consent from their patients.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. Shinal v Toms, J-106-2016, Supreme Court of Pennsylvania, Decided: June 20, 2017.
2. Valles v Albert Einstein Med. Ctr., 805 A.2d (PA, 2002).
3. Informed-consent ruling may have “far-reaching, negative impact.” AMA Wire, Aug 8, 2017.