There seems to be a never-ending stream of new tools designed to boost medication adherence. From information/support systems to physical reminders to phone apps using artificial intelligence, the list goes on and on. But before committing to any of these programs, a product manager would do well to examine the strength of the data supporting them. Better yet, back up one additional step and check the published literature showing which adherence barriers are actually the most common, and start your adherence-boosting efforts there. Let’s see what the research shows.
In Annals of Internal Medicine, Shrank and colleagues from Harvard and CVS Caremark reported on what may be the first study to comprehensively evaluate the phenomenon of prescriptions abandoned at the pharmacy.1 The study examined more than 10 million scripts in an exhaustive range of drug classes from antipsychotics to antihypertensives to antidepressants. Compared with scripts with no co-pay, scripts with co-pays of $40 to $50 had a 3.40 times greater probability of being abandoned, and those costing more than $50 had a 4.68 times greater probability of being abandoned. In the end, the authors concluded that patient co-pays “were the strongest predictors of abandonment, suggesting that patients experience ‘sticker-shock’ at the pharmacy and choose not to fill those prescriptions.”
Other recent work confirms these findings. From Health Education Research, Polinski and colleagues from Harvard Medical School, Brigham and Women’s Hospital, and Informed Medical Decisions Foundation studied primary medication adherence (PMA), which is the proper filling of the first prescription for a new medication.2 The first-noted barrier to PMA was out-of-pocket medication cost. The authors conclude that a trusting patient-provider relationship, shared decision-making support, full disclosure of side effects, and cost sensitivity are attributes that might enhance primary adherence. Further corroboration of the idea that lower patient costs boost adherence comes from multiple published studies.3-5
But in many ways, the battle against cost-based nonadherence actually begins before a patient even gets to the pharmacy; it starts in prescribers’ offices. A recently conducted survey of 363 MDs, DOs, NPs, and PAs assessed the frequency with which prescribers face patients’ drug affordability challenges. Amazingly, over three-fourths of respondents reported altering their choice of brands at least once a week due to affordability concerns, and more than a third do so at least once a day. But prescribers don’t take these affordability and access challenges lying down. They are actively searching for mechanisms to help patients gain access and reduce out-of-pocket costs. And one of the tools they lean on is manufacturer-sponsored co-pay reduction programming. Indeed, 80% of respondents agreed that co-pay coupons are an effective affordability tool.
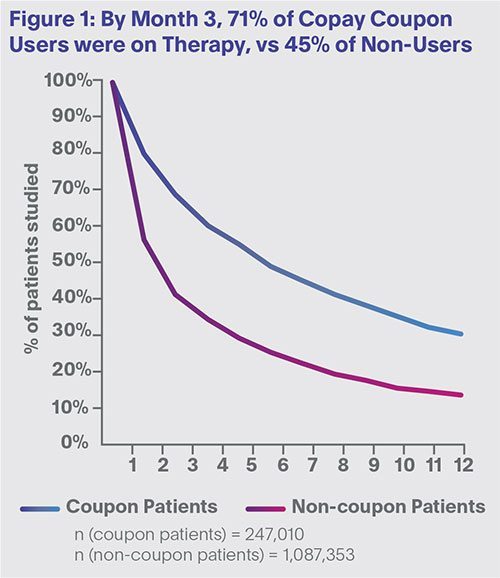
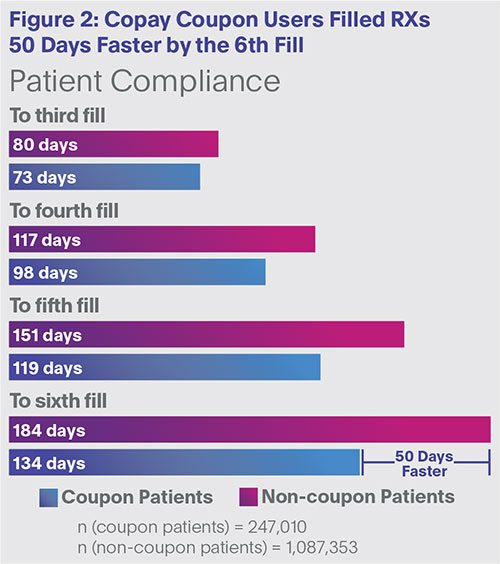
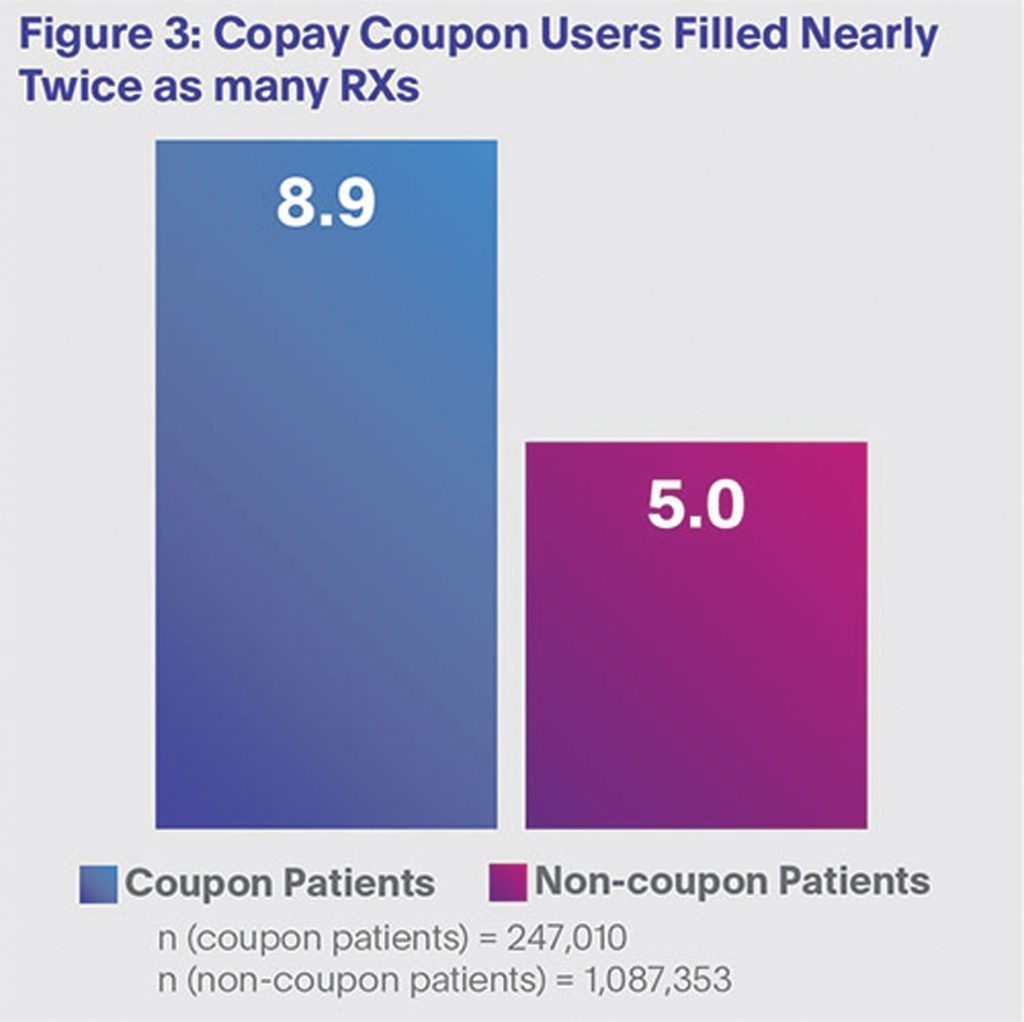
In an effort to determine the patient-adherence value of offering co-pay support, in early 2017 we compiled adherence data from 13 different co-pay programs for 12 brands across multiple therapeutic categories, including cardiovascular, endocrine, and neurological. This analysis included 247,010 co-pay coupon users and 1,087,353 non-users.
Key Finding #1: Lower Cost = Higher Persistence
First, as shown in Figure 1, a persistency gap between co-pay coupon users and non-users opened almost immediately. In fact, by month three, 71% of coupon users were on therapy vs. just 45% of non-coupon users. Moreover, this 20% to 25% adherence gap was maintained over extended months. These results corroborate earlier published data showing that patient out-of-pocket cost is a primary component of medication persistence.
 Key Finding #2: Lower Cost = Faster Speed to Fill
Key Finding #2: Lower Cost = Faster Speed to Fill
Second, patients using co-pay coupons filled Rxs 50 days faster by the sixth fill (Figure 2). On average, starting at the third fill, coupon patients filled their prescriptions sooner than non-coupon patients. Faster fills suggest greater adherence to prescribed therapy.
 Key Finding #3: Lower Cost = More Rxs
Key Finding #3: Lower Cost = More Rxs
Third, co-pay coupon patients filled more Rxs vs. non-coupon patients during the study periods (Figure 3). In fact, compared with non-users, coupon users filled nearly twice as many Rxs (8.9 vs. 5.0), providing more evidence that co-pay programs help patients get on and stay on prescribed therapy.
 So What?
So What?
What’s a brand team to do with this information? Three ideas emerge:
- Provide prescribers information about your brand’s cost status, including formulary coverage, tier position, etc. Prescribers care about patients’ drug costs.
- Provide Co-pay Assistance. Although it may seem painfully obvious, this is clearly the most salient take-away. These data provide clear evidence that co-pay programs increase compliance and extend persistence.
- Measure Program Results. The days of unmeasured efforts are over. Challenge your team to continuously test and assess your co-pay programs to ensure they are providing the impact you need and expect.
To summarize, medication nonadherence is a multifaceted problem that defies easy solutions. But despite the complexity, one lesson is clear: Adherence can be boosted by reducing patients’ out-of-pocket costs. And while reducing co-pays is certainly not the only answer to the adherence challenge, it is an important first step.
References:
1. Shrank W, et al. “The Epidemiology of Prescriptions Abandoned at the Pharmacy.” Annals of Internal Medicine. 2010 Nov 16; 153:633.
2. Polinski J, et al. “A Matter of Trust: Patient Barriers to Primary Medication Adherence.” Health Education Research. 2014 Oct;29(5):755-63.
3. Daugherty J, Maciejewski M, and Farley J. “The Impact of Manufacturer Coupon Use in the Statin Market.” Journal of Managed Care Pharmacy. 2013;19(9):765-772.
4. Starner C, et al. “Specialty Drug Coupons Lower Out-Of-Pocket Costs and May Improve Adherence at the Risk of Increasing Premiums.” Health Affairs. 2014;33(10):1761-1769.
5. Daubresse M, et al. “Effect of Prescription Drug Coupons on Statin Utilization and Expenditures: A Retrospective Cohort Study.” Pharmacotherapy. 2017;37(1):12-24.




