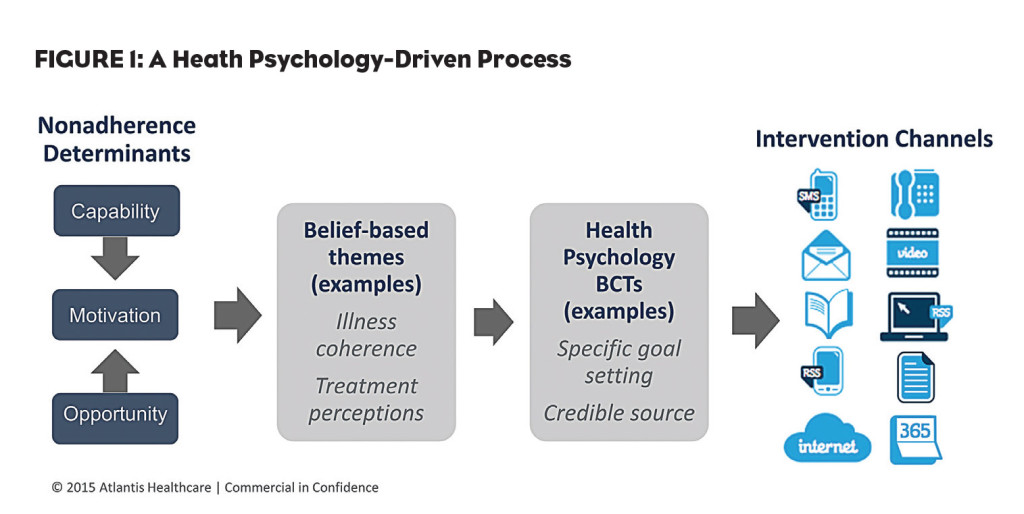
Health Psychology approaches are used increasingly for addressing treatment non-adherence across all types of diseases. A central aspect of this approach is that we look to change beliefs that drive behaviors, as these individual beliefs are proven to be more predictive of individual behavior than is the specific condition or diagnosis. Likewise, the channel for delivering patient support really is determined by what the research indicates is the most relevant channel for that person, not the disease.
This key insight is critical to understanding the relevance of health psychology not only in addressing adherence, but also in our everyday lives.
The Everyday Value of Health Psychology
We tend to talk about health psychology and behavior change as novel ideas to be used in special circumstances, but in reality we use them in many situations on a regular basis. Exercising more, eating differently, reducing stress, scheduling regular dental checkups and other “simple” acts require us to think differently and develop a plan to make a change. It can involve basic steps like deciding the benefits of an activity, writing out an action plan, or creating pro and con lists. Without even knowing it, we use the principles of health psychology and behavior change techniques to determine why we may want to make a change, how to begin the process of implementing it, and (hopefully) a plan for maintaining it for the long term.
Health Psychology Models in Practice
The beauty of health psychology and the models we use to address adherence challenges is that they are broad enough to be applicable across all diagnostic conditions and treatment categories. For example, addressing medication adherence for treatment of diabetes will involve facets of capability, motivation and opportunity. Similarly, these constructs from the COM-B model can be used in looking at a broad range of conditions including asthma, osteoporosis, cancer and rare disease.
Another frequently used model is the theory of planned behavior, which looks at constructs including attitude, perceived social norms, behavioral intention and perceived control. Like COM-B, this can also be applied across diagnostic categories, yielding different factors and providing us with a map of potential adherence challenges for the population, which can then be applied to individuals. Couple this with an analysis of other lifestyle factors that may impact an individual within the population and you have the foundation of an adherence program.
Learning Through Relevant Engagement
Experts in adult education tell us we learn best through problem-solving approaches. Simple didactics aren’t sufficient. The adult learner needs to be engaged. We also know adult learners are internally motivated, meaning they are less likely to learn when they feel solutions are being imposed on them. Rather, they need a practical, relevant approach to a problem. Thus, for every individual there will be not only preferred channels and tools that work best, but those channels and tools may differ from situation to situation, or over time. Fortunately, the behavior change techniques we use provide ample tools in a variety of styles. Conveniently, these tools can also be used through a range of channels including email, SMS, live one-to-one interactions, interactive web-based activities, group learning, social platforms, phone-based support, etc.
The key to implementing these insights in a meaningful way in addressing adherence is to recognize that everyone will leverage different techniques in different ways at different points in time. Just as we don’t all use the same process each time we try to do something new or different, we can’t expect anyone else to always use (or want to use) the same process.
Applying some basic behavior change techniques (pro/con, goal setting, and action planning) to different situations (exercise, diet, stress) with different adherence challenges (treatment concerns, treatment necessity, illness coherence), we can see that it becomes a process of mix and match (see Figure 1).
The Art And Science of Behavior Change Techniques
Research tells us that some behavior change techniques are better suited to certain populations. Similarly, certain interventions and delivery channels are better suited to specific populations, disease and treatment states. Much research has been done in this area—especially for broad health-related topics such as weight loss.
Given that we know some techniques may work better for some adherence issues and variety is critical for reaching a range of individual’s preferences, we need to have multiple behavior change techniques ready for use in each situation. These can then be applied to an array of channels to further customize the experience for the learner. Let’s look at type 2 diabetes as an example. A review of web-based diabetes management programs shows that the most common behavior change techniques used in diabetes self-care include providing:
- Feedback on performance
- Information on consequences of behavior in general
- Information on consequences of behavior to the individual
- Teaching barrier identification/problem solving
- Prompt self-monitoring of behavior
A quick literature review demonstrates a wide variety of offerings, beyond web-based self management, are available for people living with diabetes and managing treatment. While it’s hard to determine without more information which are based on health psychology and grounded in theory, the plethora of programs, channels and techniques bolsters the concept that there needs to be different strokes for different folks.
By using all of the health psychology theories and models at hand, we can paint a comprehensive picture of a disease state or therapeutic category. Mapping these onto relevant behavior change techniques and ultimately into channels, we can see the path to developing an adherence program. Once they are understood, this approach is not only practical, but intuitive and systematic, leading to a best-practices scientific approach for improving adherence over the long term, across all conditions.