Predictive Analytics Drives Coverage Gap Awareness at Point of Care
OptimizeRx
Contact Person:
Maria Cipicchio, SVP Marketing
mcipicchio@optimizerx.com
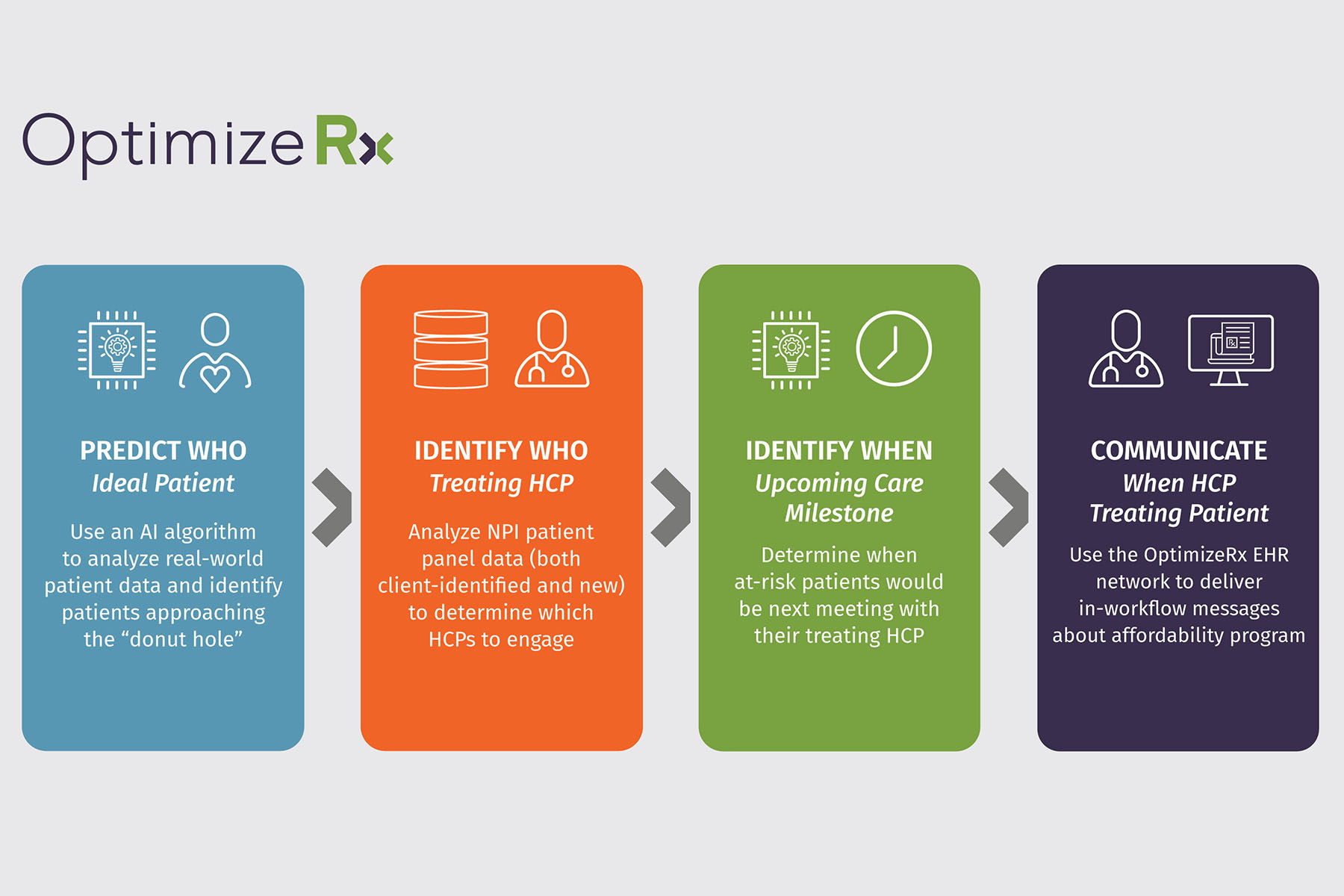
Pharmaceutical manufacturers are often challenged with anticipating and communicating with a physician before their patient enters a prescription coverage gap. OptimizeRx saw an opportunity to identify patients at risk of therapy discontinuation due to gaps in Medicare coverage by using real-world evidence (RWE) and AI to predict future care events and treatment needs of patients. OptimizeRx helps identify patients who need assistance and then enables life sciences companies to reach physicians treating those patients at the point of care through EHR messaging with financial assistance options.
OptimizeRx first launched this strategy with a life sciences partner in late 2021 and have continued to improve and build on it in 2022, delivering initial results on the active program in June 2022. Working with the pharmaceutical manufacturer, they were able to identify patients with a chronic illness who were approaching the Medicare coverage gap and were likely to experience an unexpected cost increase within a week’s time. The model also predicted the next time the patient was likely to see their provider. The platform messaged the physicians before their patients hit the coverage gap so that the provider had affordability options to offer their patients and help them avoid costly prescription increases or non-adherence.
Results over a six-month period for the brand include 46,000+ incremental scripts among HCPs receiving affordability information and financial resources for their patients and 27% of the HCPs identified and targeted for the affordability information enrolled a patient for the first time. Additionally, the program represented a 200% growth over the manufacturer’s initial number of HCPs identified with “at-risk” patients.