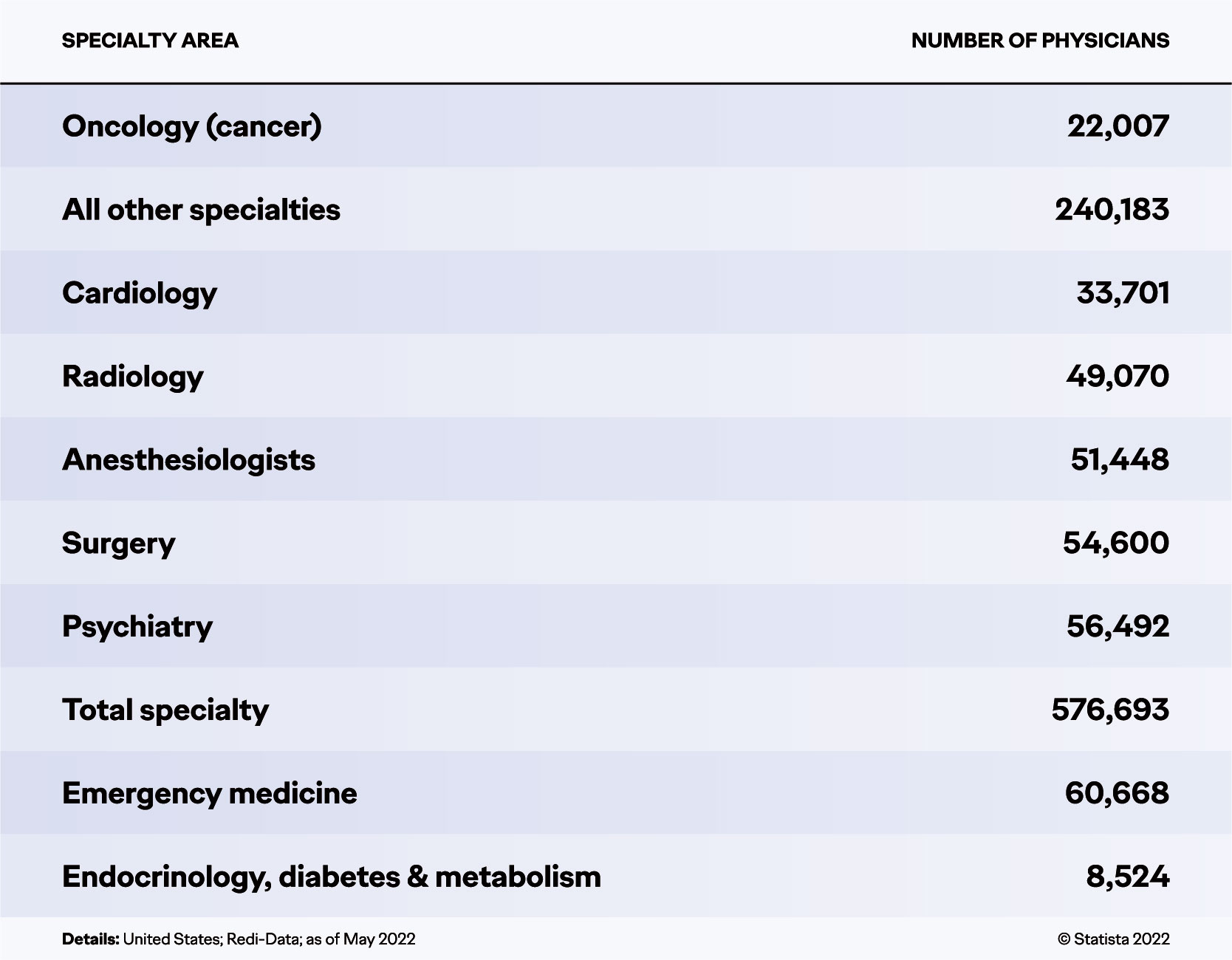
For several years, the American Society of Clinical Oncologists (ASCO) has published what they call an annual “Snapshot: The State of the Oncology Workforce.”1 According to these reports, the proportion of oncologists aged >64 years/nearing retirement has steadily increased (19.7% in 2020, 21% as of 2022) while the proportion of those aged <40 years/new to the profession has steadily diminished (15.6% in 2020, 13.9% as of 2022). And according to Statista, numbers of oncologists are the second lowest in medical subspecialties in America (following endocrinologists) even though cancer is second only to heart disease as this country’s most common cause of death (see figure below).2
 Arguably, oncology is one of the top five most difficult medical specialties to pursue; going into it means knowing that a substantial number of your patients will die. While surviving a cancer diagnosis in America rose 32% between 1991 and 2019 (ASC 2022), oncologists have only one professional certainty—that the disease they treat is unpredictable; when and where it will progress from one body system to the other remains a relative mystery.
Arguably, oncology is one of the top five most difficult medical specialties to pursue; going into it means knowing that a substantial number of your patients will die. While surviving a cancer diagnosis in America rose 32% between 1991 and 2019 (ASC 2022), oncologists have only one professional certainty—that the disease they treat is unpredictable; when and where it will progress from one body system to the other remains a relative mystery.
So, what leads young doctors to dedicate their careers to patients for whom there may be no cure? Or to guide them through treatments that are usually more painful than the disease? Wanting to better understand what drove them emotionally and intellectually, Ogilvy Health interviewed 12 oncologists last June about their profession. We supplemented learnings from these interviews with a range of data available online, studies exploring similar terrain.
Looking at the effect of COVID-19, current market dynamics, and a range of other pressures facing today’s oncologists, here’s what we found: a culture of professionals embracing their essential role within a high stakes arena. It’s a job where every choice made with and for a patient can have deep consequence. It means navigating rising numbers of patient comorbidities that can potentially exacerbate any cancer care. It demands responsibility to maintain a perpetual eye out for relevant new treatment developments while operating within a medical arena experiencing a plethora of trials and research. What follows is a brief exploration of the professional identity of oncologists.
The Inspiration for Oncologists
Among several of the oncologists we interviewed, initial interest in the specialty (indeed all of medicine) was ignited by an early experience with cancer—someone they knew having suffered from it. But even for those who did not mention such experiences, the discipline seemed highly personal. The daily face time helping patients with cancer to navigate the disease seems core to their identity. Asked about what most inspires them in their daily work, most talked about the interactions with patients (and often family), however materially inadequate their ultimate efforts may be.
“Obviously, we lose a lot of oncology patients but even there, the ability to transition them from a period of care to supportive care, the bonds that you’ve formed are very gratifying,” one oncologist told us.
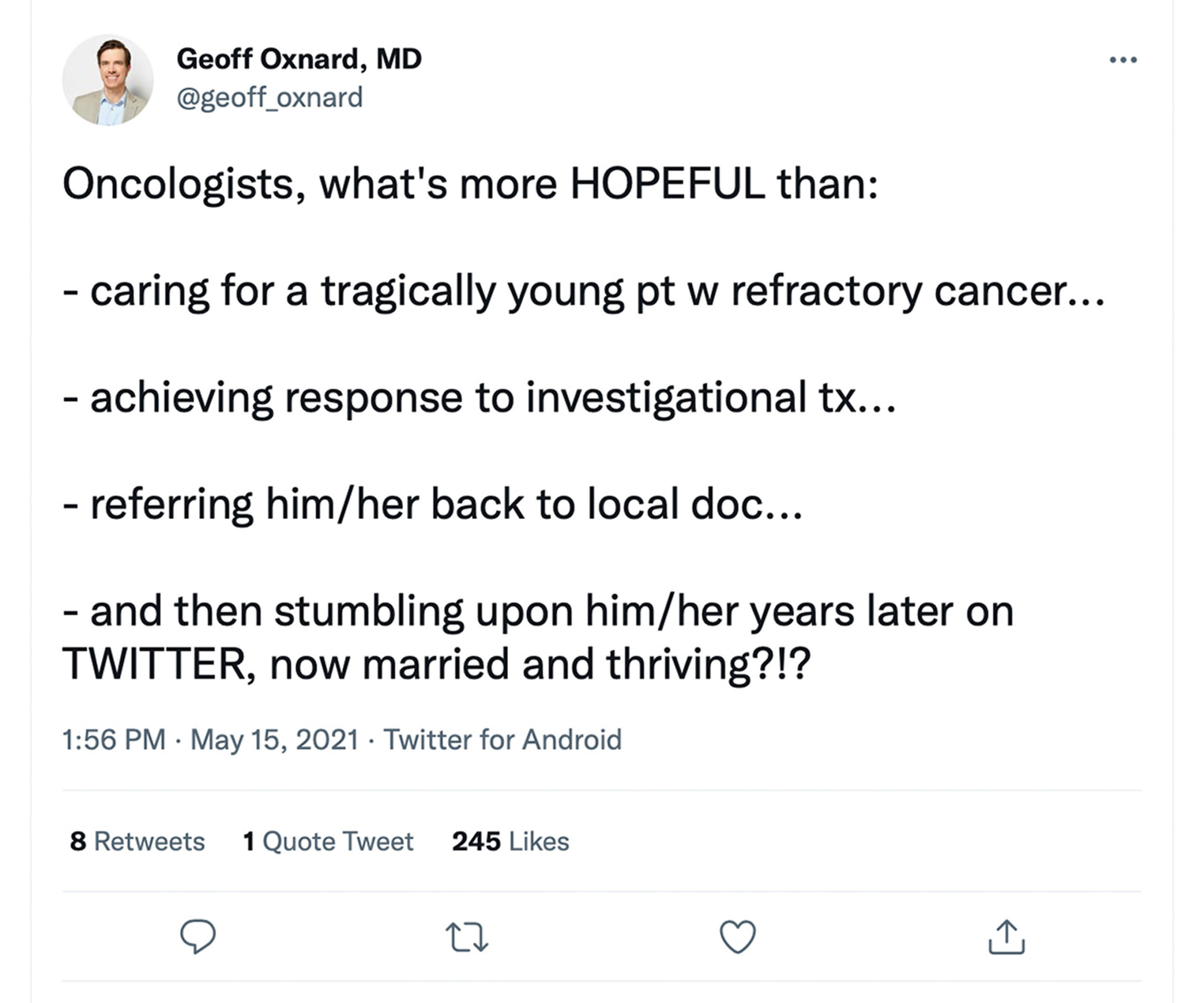
Consider that bond. The diagnosis arrives with an intrinsically unpredictable prognosis. Patients inevitably require hand holding. Oncologists can’t prescribe hope, but they can keep it alive (see tweet below). The job demands sophisticated listening skills and the ability to balance compassion with composure. High levels of emotional engagement are the essence of “cancer care.”
 “It’s not a procedure-oriented specialty as, say, in cardiology or in GI. If you are especially into cardiac cath or you’re into doing endoscopy, you pretty much do the procedure and are not very involved with the patients before and after. Here, you form a bond, which is, at least for my personality, something which is very gratifying.”
“It’s not a procedure-oriented specialty as, say, in cardiology or in GI. If you are especially into cardiac cath or you’re into doing endoscopy, you pretty much do the procedure and are not very involved with the patients before and after. Here, you form a bond, which is, at least for my personality, something which is very gratifying.”
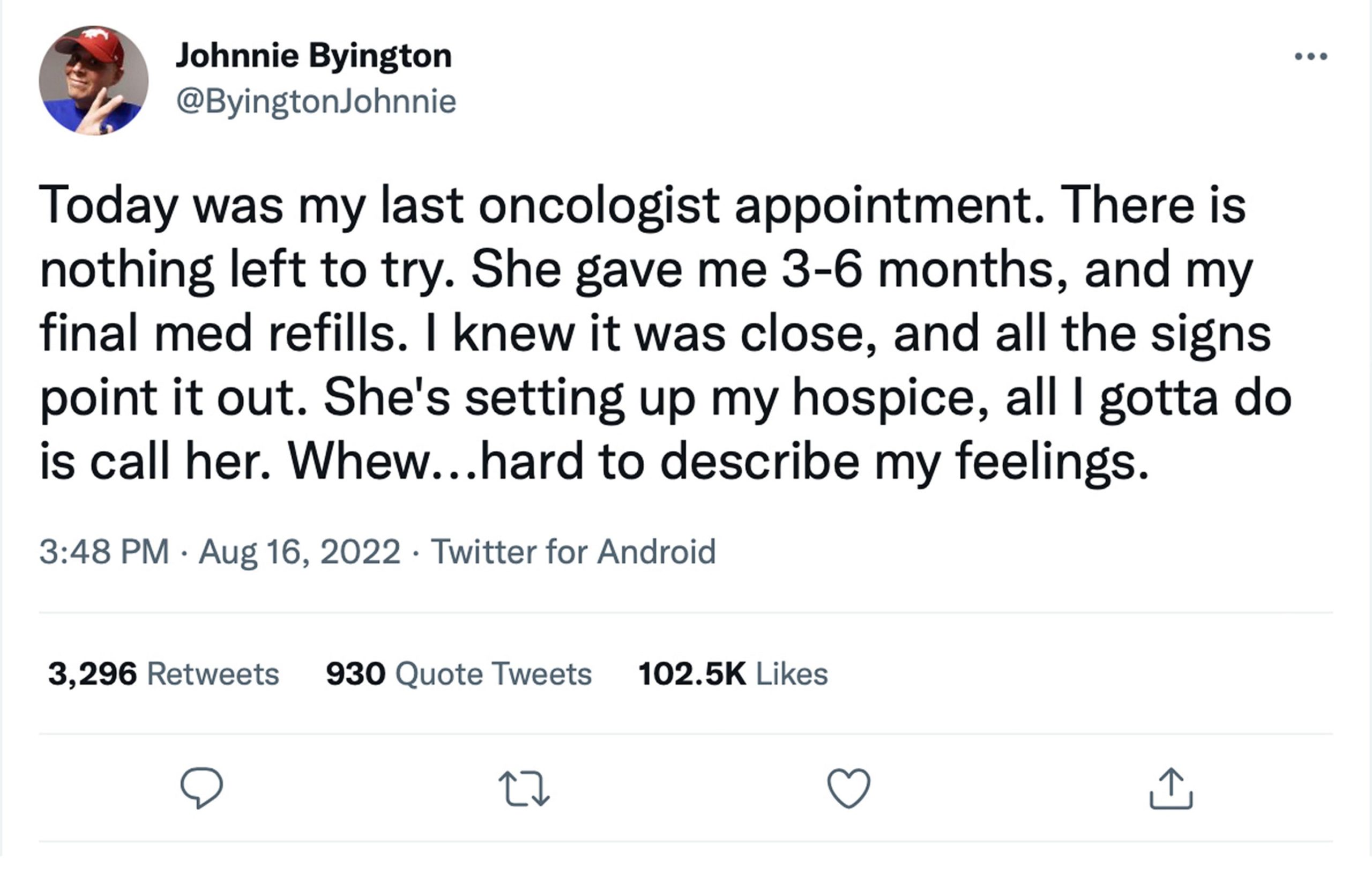
Ultimately, the oncologist acts as a patient guide on medical, emotional, and spiritual levels, often simultaneously. As one oncologist put it, “you’re an oncologist, you’re a critical care doc, you’re a generalist. You wear many hats.” There’s a humility in how oncologists talk about those hats. Indeed, the oncologist community seems energized by sharing stories around the challenges of the practice, from the promise and limits of medical science to honoring patient input as these individuals face possible or certain death (see tweet below).
 Keeping Up with Treatment Innovation
Keeping Up with Treatment Innovation
Every issue of the Journal of Clinical Oncology publishes “the Art of Oncology,” a section dedicated for stories from practitioners about their daily practice. Far from dark or depressing, published oncologist narratives resonate with verve, even humor.
For an example, look for the stories from oncologist Dr. James Swalz. Between 2011 and 2017, his blog “Sunrise Rounds” detailed life in the trenches of caring for patients with cancer. His September 10, 2014 entry was titled, “What’s It Like to be an Oncologist?”3 In it, Dr. Swalz highlights one day:
7:00 am Lights on.
Coffee, black and a banana. Paperwork. 27 patient visits, 3 emergencies, 35 phone calls. Lots of computer time. Some laughs and a few tears. Paperwork. Last family meeting. Coffee, black. In between: Thursday.
Tears. Laughter. People. Paperwork. In between exists the perpetual need to keep up with the latest cancer research and innovations—no casual endeavor. Access to the most relevant treatments and patient trials is essential to the oncologist-patient partnership, the potential difference between stopping a cancer metastasizing or not. That’s an immediate demand for knowledge that any company involved with serving the oncology market needs to address.
There’s a plethora of those companies. According to “Global Oncology Trends” (a study published this year by the IQVIA Institute for Human Data Science), 2021 saw the highest number of cancer trial starts, “up 56% from 2016…”4 The same year, American oncologists worked in a market that saw the emergence of “20 new cancer medicines and two cancer diagnostic agents….” IQVIA’s study reports that since 2011, “55 unique new hematological cancer medicines” have launched.
Oncology is a medical discipline where keeping up is critical. Traditionally, oncologists looked to big pharma for such informational needs. But as outlined in IQVIA’s study, 68% of new cancer treatments are from emerging biopharma companies, organizations that lack the resources to spend on strong outreach to oncologists.
In the interviews we conducted, oncologists talked about the value of long-lasting personal relationships with pharma leadership, from the scientists to the sales teams. Emerging biopharma companies would be wise to start outreach, and larger companies should continue to explore how to strengthen these relationships, especially soliciting input on trials, easier access to new patient treatments, and education on the relevance of new innovations and research.
More Challenges and Changes in Oncology
Staying current on new trials and treatments is just one of multiple obstacles oncologists confront. In 2018, ASCO published an analysis of surveys taken among oncologists between 2013 and 2017, including polls about practice challenges.5 The top issue between 2015 and 2017 was payer pressure, primarily around prescription coverage (prior authorizations followed by coverage denials). Three years later, another excellent study fielded by Amplity Health and online social network SERMO, found patient medical costs still rated high among concerns.6 But even higher among everyday practice challenges was what the study termed hectic professional schedule. Reading the study’s verbatims, what you hear are oncologists concerned about ever-diminishing time to spend with their patients.
What changed? More patients diagnosed with cancer. Equally challenging, the study found, patients now arrive with more comorbidities, which invariably complicate treatment options and approaches. In addition, oncologists increasingly work within larger practice settings such as hospitals and networks with bottom-line focused protocols demanding they see more patients. These demands inevitably cut into the qualities that inspired so many oncologists to pursue the field—the one-to-one patient interaction.
Overall, our oncologist interviews pointed to recognition that their roles are in transition; rather than acting as stewards at the helm of the patient’s journey, oncologists are on a path to serving as more equal members of a larger crew. Already, nurse practitioners and physician assistants are providing increased patient care. Payers and hospitals increasingly play a bigger role in treatment decision-making.
The challenge for any organization serving oncologists is how to tap into the existing experts. As older oncologists retire, this sector may lose a wealth of institutional knowledge. Simultaneously supporting new generations of professionals in cancer care is also important. Smart pharma and biotech brands will partner with today’s oncologists for their knowledge, commitment, and passion, and help elevate all those just entering the profession.
Concretely, that means devoting resources to building a high-quality depth of infrastructure to support oncologists and oncology. That translates to culling first-rate talent among service, sales, marketing, and communications teams, not to mention seeking ways to solicit oncologist input on innovating toward a future where cancer won’t disappear but surviving it will mean ongoing care. A world in which companies developing the next-generation treatments will still benefit from strong relationships with oncologists, a profession where scientific knowledge and empathetic sensitivity are two sides of the same coin—the human capital of cancer patient advocacy.
References:
1. ASCO. “State of Cancer Care in America.” Accessed August 25, 2022. https://www.asco.org/research-data/reports-studies/state-cancer-care-america.
2. Statista.com. “Number of Active Physicians in the U.S. in 2022, By Specialty Area.” Statista.com website. Accessed August 25, 2022. https://www.statista.com/statistics/209424/us-number-of-active-physicians-by-specialty-area.
3. Swalz J, “What’s It Like to be an Oncologist?” KevinMD. Accessed August 25, 2022. https://www.kevinmd.com/2014/09/whats-like-oncologist-just-one-day.html.
4. IQVIA. “Global Oncology Trends.” https://www.iqvia.com/insights/the-iqvia-institute/reports/global-oncology-trends-2022.
5. Kirkwood MK, Hanley A, Bruinooge SS, et al. “The State of Oncology Practice in America, 2018: Results of the ASCO Practice Census Survey.” J Oncology Practice. 2018;14(7):e412-e420.
6. Amplity Health, 2020. “Understanding Oncologists: A Detailed Examination of Practice Pressures and Desired Interaction with Pharma Manufacturers.” Accessed August 25, 2022. https://www.amplity.com/images/wpuploads/2020/09/A-Detailed-Examination-of-Practice-Pressures-and-Desired-Interaction-With-Pharma-Manufacturers-.pdf.










