It has long been understood that cancer cells have a different metabolism from that of normal cells, but this was widely thought to be a by-product of the genetic alterations that are the suspected drivers of cancer development.
Though early proponents of tumor metabolism argued that cancer was fundamentally a metabolic disease, this idea was sidetracked as we entered the genome-sequencing era and focused on precision medicine. In the past decade, however, we’ve come full circle as many researchers have again begun to advocate for a revival of the idea that tumor metabolism might represent a root cause of cancer.
“Altered metabolism can be both a cause and an effect that is essential for cancer progression,” Dr. Chi Van Dang, director of the Abramson Cancer Center at the University of Pennsylvania, Philadelphia, said in an interview.
Cancer’s sweet tooth
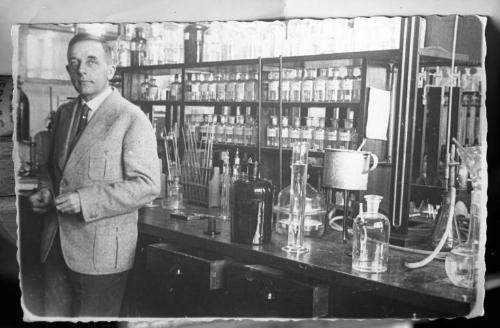
The unique metabolism of cancer cells was first highlighted almost a century ago by the German physiologist Dr. Otto Warburg. He noticed that cancer cells change the way they derive energy from glucose. Typically, cells use glycolysis to convert glucose into pyruvate in the cytoplasm. The pyruvate is then fed into the mitochondria to produce energy through oxidative phosphorylation, which requires oxygen. When oxygen levels are low, cells are able to make energy through glycolysis, but this is much less efficient, yielding far less energy for each glucose molecule consumed.
Cancer cells, however, seem to prefer to use glycolysis, even when oxygen is plentiful, and in order to compensate for the fact that glycolysis produces significantly less energy, the cancer cells take up much more glucose than their normal counterparts.
Dr. Warburg’s rationale was that cancer cells use glycolysis because their mitochondria are damaged, and he even proposed that this defect was “the root cause of cancer,” that the genetic dysregulation of cancer cells could be traced to impaired respiration and energy metabolism. In fact, it turned out that mitochondria, for the most part, are intact in cancer cells, and, because the “Warburg effect,” as it has come to be known, didn’t fully explain how cancer develops, it was written off as an effect of cancer, rather than the cause.
Beyond the Warburg effect
As we have added to our understanding of how cancer develops, it has become increasingly clear that many of the drivers of tumorigenesis are intricately linked to cellular metabolism, which has renewed interest in Warburg’s hypothesis and in tumor metabolism.
Because the Warburg effect didn’t appear to be an adaptation to defective respiration, the question remained as to why cancer cells would use a less efficient method of energy production. The answer, at least in part, is that they aren’t just using it to make energy.
Cancer cells are growing and dividing very rapidly, and they need a quick and efficient means of producing all of the metabolic building blocks they need to do this. Using glycolysis is a trade-off between making less energy and making it more quickly. Furthermore, the conversion of glucose into pyruvate via glycolysis occurs through several intermediates that can be diverted into other biosynthetic pathways that produce some of those much needed building blocks required to produce essential cellular components.
Although the Warburg effect is still the best characterized metabolic distinction in cancer cells, it can now be added to a growing number of dysregulated metabolic processes.
“Cancer’s sweet tooth is not the entire picture,” said Dr. Dang, “because cells are made of more than just carbon, hydrogen, and oxygen.” Research has shown that there is a fundamental change in the metabolism of all four major classes of macromolecules – carbohydrates, proteins, lipids, and nucleic acids. Cancer-associated alterations have been shown to encompass all aspects of cellular metabolism, increasing the ability of tumors to acquire nutrients, but also dictating how those nutrients are used.
As the understanding of tumor metabolism is growing, so too is an appreciation of its heterogeneity. Not all tumor types and, indeed, not all cells within the same tumor, will display the same metabolic profile. The metabolic needs of a tumor can depend upon nutrient availability, the influence of its surrounding environment, and the distance to the nearest blood vessels.
The selfish cell
Many researchers have also begun to reexamine the idea that tumor metabolism is more than just a hallmark of cancer. On the one hand, Dr. Dang explained, “there are mutations in genes that affect mitochondrial function that leads to cancer and in metabolic enzymes that in turn trigger cancer development through altering the epigenome.” On the other hand, “cancer genes – oncogenes and tumor suppressor genes that drive cancer development – can alter cancer cell metabolism to support cancer cell growth.” Hence, one can argue for a role of tumor metabolism as both a cause of tumor growth and one of the many effects of the genetic mutability of cancer.
An example of a widely studied gene that has turned out to be vital to tumor metabolism is the MYC oncogene that encodes a transcription factor with a well-known role in cell cycle progression. It turns out, said Dr. Dang, that “MYC opens up the fuel line to drive cell growth; it drives genes that import nutrients into cells and metabolize nutrients to make the building blocks for the growing cell.”
Many of the growth factor signaling pathways that are commonly dysregulated in cancer don’t just regulate cell growth and proliferation, but are also intimately involved in dictating the response to nutrients. A prominent example is the PI3K/Akt pathway; among the most highly mutated pathways in human cancer, it acts as a master regulator of glucose uptake.
Some researchers propose that alterations in growth factor signaling pathways drive cancer formation because they allow the cell to flaunt the rules of the dinner table. Essentially, instead of acting like a cell that forms part of a multicellular organism, taking cues from the surrounding cells about when and how to respond to nutrients, cancer cells are able to ignore these signals and take up whatever nutrients they can find. This may also explain the observation that cancer development is closely linked to obesity and diabetes.
Targeting metabolism
These discoveries have led researchers to consider the possibility of targeting metabolism to prevent cancer cell growth. Some commonly used chemotherapy drugs have a metabolic mechanism of action; the antifolates methotrexate and pemetrexed, for example, target one-carbon metabolism.
Although no metabolism-based small-molecule drugs are approved yet, many are in preclinical development, and some are beginning to move forward into clinical trials. Dr. Dang highlighted the development of drugs targeting metabolic enzymes: “Drugs being developed against the mutant enzymes IDH1/2 have demonstrated clinical responses in acute myelocytic leukemia, and other drugs, such as CB-839 – an inhibitor of glutaminase – are undergoing clinical studies.”
Several existing drugs have also been repurposed in the fight against cancer, including some not previously thought of in this context, such as the antidiabetic drug metformin, which has shown significant promise. Dr. Dang concluded: “The future outlook is the generation of a new class of drugs that could, in combination with other drugs, result in better clinical treatments for cancers.”