Novo Nordisk is using its digital health portfolio to not only provide resources for patients and providers, but to also conduct research to uncover real-world data that can help them even further. At this year’s American Diabetes Association Scientific Sessions (ADA) in June, the company presented findings from a study conducted using self-reported patient data from Novo’s Cornerstones4Care® Powered by Glooko app. The study, conducted over a 14-day period with 112 type 1 diabetes patients, examined the association between variations in blood sugar levels and the amount of time spent with low blood sugar levels.
PM360 spoke with Todd Hobbs, MD, Vice President and Chief Medical Officer of Novo Nordisk about the results of the study, what else the company might study using the app, how they plan to use the data they collect to help patients, and how the growing importance of real-world data is changing how the company operates.

PM360: Can you explain the methodology behind the study you did using the Cornerstones4Care Powered by Glooko app. How did you choose the patients you were getting the data from?
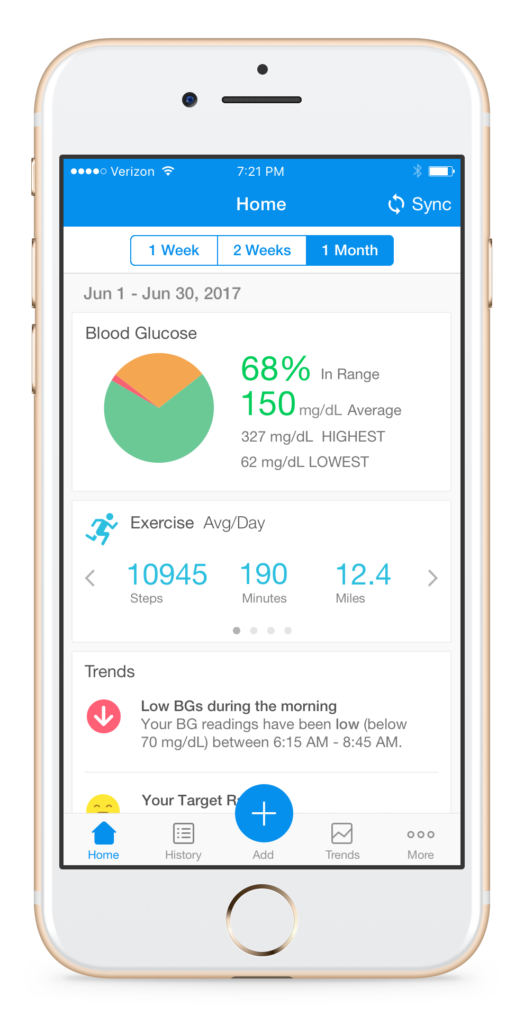
Todd Hobbs: We don’t choose the individuals who respond. Cornerstones4Care is a comprehensive patient support platform that provides a broad range of diabetes management tools and resources such as meal planning, medication tracking, coaching support from a Certified Diabetes Educator, etc. Patients using the Cornerstones4Care powered by Glooko app can self-report their type of diabetes, age, gender, and medications. Additionally, the app syncs with most blood glucose meters, insulin pumps, and continuous glucose monitors, in addition to many fitness trackers such as Fitbit and Moves.
When we pulled data for the poster, we had about 5,482 patients who had downloaded the app. We then narrowed it down from there. For this particular study we wanted to look at type 1 patients, so those who had self-reported that they were diagnosed with type 1 diabetes versus type 2. That took us down to more than 600 patients. But, for this particular research we wanted those individuals who had continuous glucose monitoring (CGM) ability. That’s how we came up with the total of the 112 patients who had type 1 and then also had the ability to submit the CGM.
Once you narrowed down the patients, why did you choose to focus on tracking their blood sugar?
Classically, we’ve always talked about how your risk for having low blood sugar—hypoglycemia—is somewhat correlated to your overall control of your A1C. And it’s always been thought that whatever you’re doing to get that A1C closer to normal, that increases your risk for having low blood sugar. But some recent data has indicated that, no, in fact there are other things involved. That individuals who have, perhaps, high A1Cs are still at a significant risk for having a hypoglycemic event.
We wanted to look at the role of the variability in the glucose—glycemic variability—and whether that influences the patient’s risk for having hypoglycemia. We wanted to confirm that other data that suggest if your glucose is high but it’s stable and you’re 200 all the time, then your risk for a hypoglycemic event is not very great. But, if your average sugar is 200 yet you’re going from 400 to 100 all the time, back and forth, and you’re having a lot of variability, then it makes sense that your risk for having an unexpected hypoglycemic event is greater.
So, what did you find?
It was pretty remarkable. We measured both the patient’s average blood sugar—if you will—and then we looked at the coefficient of variability from that average. And there are some CGM standards from a committee that say if you have roughly over about 30% of variation from your mean, that increases the risk for having a low blood sugar event. And clearly, as the poster reported, that’s what we found. The more variability that was had—or the more that coefficient of variability moved away from that 30% even as up high as about 50% variation—that increased the risk for an individual to have a low blood sugar of less than 54. Certainly, when someone is less than 54, those are serious events. That would cause a person to have both mental capacity changes in thoughts and also physiologic changes, and it needs to be treated pretty quickly or it could lead to even further problems such as seizure.
The other thing we found was the risk for having these hypoglycemic events was not actually as much correlated to the A1C or to the average glucose level. It was really more correlated to the coefficient variability or the increase in variability more than it was to their overall control. So, again, it does support the recent research suggesting that your risk for hypo is really not as much correlated with your overall control as it is the variability.
Now that you’ve found that, is there anything you can do to utilize that information to better help patients either through the app or through other measures?
Yeah, there are a couple ways. Obviously, the individual patients who can see their own patterns through the Cornerstones4Care powered by Glooko app can get some immediate feedback, such as, “Hey, maybe pay close attention to this time of day.” But really, we want to get this data out there because in the U.S. there are many endocrinologists who are very comfortable with type 1 diabetes patients, but many of the primary care physicians may not be as comfortable with downloading meters, and sensors, and day-to-day management. So, increasing the awareness of the fact that even though a person’s A1C may be okay, or even kind of high, you still need to be asking about whether or not they’re having a lot of variability in their glucose from a day-to-day perspective. After we raise awareness, then we can further explore the factors that may lead to some of this variability. Maybe it’s the patient’s activity. Maybe they need to consider the timing of their insulin or the specific products. Those things we’ll do as we follow up.
Are there any other studies you’re planning to use the app for to find any more learnings that you’re curious about?
Yeah, the beauty of this app is that we’re going to learn a lot as we go along. What we’re doing now is collecting the data. So, after we have a lengthier time period to collect some of the data, we’re going to start looking at what are the right questions to ask? How much are the patients entering their medications? How much information we’re getting on individual’s control? But right now, we’re still in the collection phase of this and getting the self-reported data just to see who’s going in there, who’s entering data, who’s using the system, and what they’re putting in, so then we can help figure out what the best information is to analyze and actually report and give back to them. However, the patients themselves don’t need to wait on the data analysis from all these sources. They get feedback almost instantly when they’re entering information that is keeping them engaged in their care.
In terms of that real-time monitoring and feedback, are patients currently getting like real-time alerts? For instance, as soon as they enter something that is a concern, are you instantly providing them with something that can help them?
It’s not quite that dynamic yet, but what will happen is that as they enter their information they will be able to see recommendations for changes in their lifestyle, or tips, or things like that. And the more engaged the person is in putting in their information, the more information they’re going to get back. For instance, I wear a pump and a meter that I use to correlate. Even the simple meter will alert me. It may say, “You know, the last three days you’ve been above your target at dinnertime.” So I know that tomorrow when I eat dinner I need to consider that maybe I need a little bigger amount of bolus or insulin. That sort of feedback is really going to be helpful.
You mentioned it wasn’t that dynamic yet. Is that something you are working towards—more immediate notifications or feedback?
The challenge there is not a “can we do it?” from a capability standpoint, but with the FDA there are regulations in regards to treatment advice. While we have many systems that have the capability to do that, it actually will need a little bit more regulatory approval to be able to give treatment advice. Ultimately, we want to connect the patients and their providers, so they can help manage many of these situations on a more active level. But we have to be careful how we do that as a pharmaceutical company and as always placing patient safety before anything else.
So then, is that where you think apps like this and real-time data provide the most value, in helping to provide that connection between patients and providers?
Yes, because clinicians have a few minutes with patients every few months. But for a patient who really wants to be engaged and wants to manage their diabetes, it’s about connection, information, and getting them information really at any time and almost every time they need it. We believe that Cornerstones4Care already offers the resources, but even using, say for instance, the Cornerstones4Care powered by Glooko app we can provide more connectivity with the patients on their own time, and again, eventually bringing that clinician in. It’s really just about connecting the individuals. We know there are many patients who don’t want to use an app, but hopefully, we can still connect with them via online resources or the other channels Cornerstones4Care provides. But for those individuals who really embrace apps and connectivity, we want to be able to provide that opportunity for them and share the information through the app with their providers.
Real-world data like this is also becoming more important for pharma companies, for purposes such as negotiations with payers. So, how else is your company using this data?
Obviously, that is a big focus of ours. As you’re probably aware, this is a growing area in the way data is reviewed in the real world. While we still have to do randomized control trials for regulatory approval for our products, it is becoming more important to understand how they work in the real world. For instance, we have a research agreement with Cleveland Clinic. And we obviously work with payers—we have to work with them. Many times, that means they want to look at their own data sets, their own population, and see how our products, treatment algorithms, or therapeutic choices work.
It’s kind of partnering with them to ask the right questions, look at the right inputs, their end-points, and to understand the data. They may have their own data collection and analyses, but we help them with looking at the right information. At the ADA this year, a huge area of discussion across the meeting was real-world data. And, real-world data has many forms.
Unfortunately, the tough part with real-world data is you need to have your products out there for a certain amount of time to get the uptakes. We’re trying to—as soon as the product is approved or launched—to have a plan in place to collect the data and then be able to analyze it as we go along. For instance, we have Ozempic® which was just recently launched in January. We’re already embarking on looking at real-world data and large health systems to see immediately what patients started it, how they’re doing, are they adhering, and if they’re not, then what are the reasons. Again, it’s just trying to find the real-world questions and best use of that data, because we very much recognize the importance of it.