EXPERT ANALYSIS AT THE 2015 JAMES W. FRESTON CONFERENCE
CHICAGO (FRONTLINE MEDICAL NEWS) – New evidence is shifting attention from low-grade inflammation to mast cell activation as a driving mechanism behind visceral hypersensitivity in irritable bowel syndrome (IBS).
Low-grade inflammation has been intensely studied as a major mechanism of visceral hypersensitivity in the gut wall ever since the observation that interleukin-1beta (IL-1b), lamina propria T lymphocytes, and enterochromaffin cells are overexpressed in patients who develop IBS following a gastrointestinal infection, according to Dr. Guy Boeckxstaens of the Translational Research Center for GI Disorders, KU Leuven (Belgium) University Hospital.
Studies have also reported increased release of cytokines by peripheral blood mononuclear cells in patients with IBS, compared with healthy controls, and that this activates afferent nerve fibers by IL-1b and tumor necrosis factor-alpha (TNF-alpha) ( Gut 2013;62:1456-65).
Though interesting findings, they have not been confirmed, and several studies have reported no difference in cytokine expression, cytokine serum levels, or number of immune cells in patients with IBS, he said.
Among them is a systemic review and meta-analysis showing no significant difference in levels of IL-10 and TNF-alpha serum/plasma levels between patients with IBS and healthy controls (Neurogastroenterol Motil. 2014 Jul;26:1036-48).
The strongest argument against a significant role for low-grade inflammation, however, lies in two recent randomized, clinical trials that found no significant overall effect on IBS symptoms with 12-week treatment with the anti-inflammatory drug mesalazine, compared with placebo in patients with IBS (Gut 2014 Dec 22. doi: 10/1136/gutjjnl-2014-308188 . [Epub ahead of print]) or diarrhea-predominant IBS (Gut 2015 Mar 12. doi: 10.1136/gutjnl-2015-309122 . [Epub ahead of print]), Dr. Boeckxstaens observed.
“On the whole, and I know I’m very provocative here, there is no or just a very minor role for low-grade inflammation in the pathophysiology of IBS visceral hypersensitivity,” he said at the conference sponsored by the American Gastroenterological Association .
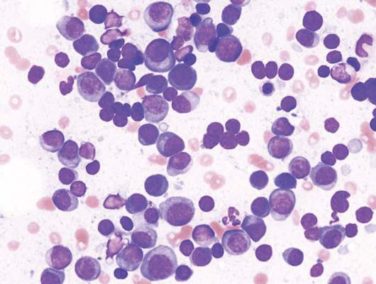
Instead, in his view, a more likely mechanism is mast cell activation, an idea first put forward in 2004. In particular, it is that mast cell activation, through release of mediators such as histamine, serotonin, and proteases, can lead to activation, sensitization, and upregulation of nociceptors, leading to visceral hypersensitivity in the gut wall. How these mast cells are activated is the “$10 million question,” Dr. Boeckxstaens acknowledged.
Stress is clearly a trigger in IBS and, at least in animal models, has been shown to induce eosinophils to release corticotropin-releasing hormone, which activates mast cells. But he posits that chronic inflammation and infection may also trigger a bystander immune response against innocent antigens.
“We all know that we have tolerance to food, to bacteria present in our gut, but an inflammatory response can interfere with this mechanism,” he said. “We reason that if you have an infection, a danger signal, that this danger signal may trigger an immune response against innocent antigens present at that moment and if you then reexpose the immune system to these antigens, you may trigger an immune response, activate mast cells, and in that way lead to afferent nerve dysfunction and increased hypersensitivity.
“It’s all very speculative, but I think it’s a very interesting new scheme,” he added.
To test this theory, Dr. Boeckxstaens and his colleagues infected Th2-background mice with Citrobacter and at the same time exposed them to ovalbumin antigen or placebo. As expected, there was an inflammatory response and increased abdominal pain that normalized after 4 weeks, but intriguingly, when they began feeding the mice again, hypersensitivity returned at 7 weeks only in the mice exposed to ovalbumin antigen during infection. Further, treatment at 7 weeks with the mast cell stabilizer doxantrazole reversed the hypersensitivity, “showing that mast cells indeed seemed to be activated if you reexposed these mice,” he said.
Dr. Boeckxstaens pointed out that a recent German study in humans fits nicely with this idea, reporting that diluted food antigens delivered directly into the duodenum caused mucosal responses in two-thirds of patients with IBS and suspected food intolerance and increased intraepithelial lymphocytes ( Gastroenterology 2014 Nov; 147:1012-20.e4 ).
Recent evidence also points to the role of upregulation and sensitization of pronociceptive receptors/channels in IBS visceral hypersensitivity. Unpublished data from Dr. Boeckxstaens’ lab using supernatant of diarrhea-predominant IBS patients show that histamine sensitizes transient receptor potential vanilloid 4 (TRPV4), TRPV1, and transient receptor potential ankyrin 1 (TRPA1) on human submucosal neurons through H1-receptor activation.
Though much of this may seem a long way from clinical practice, he observed that 12-week treatment with the histamine-1 antagonist ebastine more than tripled the percentage of IBS patients with at least considerable relief of IBS symptoms, compared with placebo in a double-blind, randomized trial involving 55 patients.
Dr. Boeckxstaens reported no financial conflicts of interest.
On Twitter @pwendl