AT THE LIVER MEETING 2016
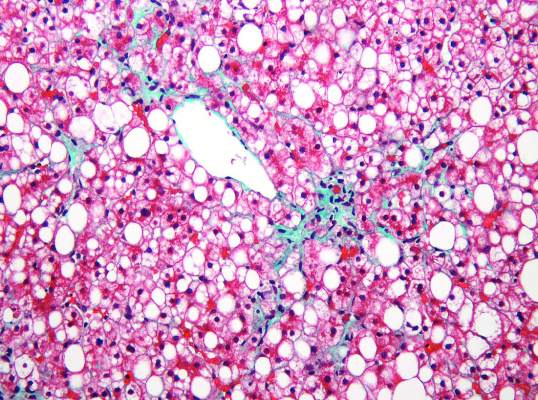
BOSTON (FRONTLINE MEDICAL NEWS) – Metabolomics of liquid biopsies noninvasively identified nonalcoholic fatty liver disease (NAFLD) with and without steatosis, and assessed the severity of both steatosis and fibrosis, Puneet Puri, MD, reported at the annual meeting of the American Association for the Study of Liver Diseases.
“These data provide proof of concept that liquid biopsy metabolomics can be used to resolve diagnostic questions in NAFLD management,” said Dr. Puri of Virginia Commonwealth University Medical Center in Richmond.
NAFLD is the most common chronic liver condition and urgently needs point-of-care diagnostics, Dr. Puri and his associates noted. Therefore, they recruited 817 patients with biopsy-confirmed NAFLD and 130 biopsy-confirmed controls from 16 centers in the United States and Europe. They divided these individuals into separate test and validation cohorts.
The researchers first developed a model that distinguished NAFLD patients from controls based on body mass index and the relative plasma concentrations of 11 triglycerides. This model correctly classified patients and controls 90% of the time (area under the receiver operating characteristic curve [AUROC], 0.90; standard deviation, 0.02) in the discovery cohort, and 93% of the time in the validation cohort (AUROC, 0.93; SD, 0.03). The sensitivity of the model was 98% in the discovery cohort and 97% in the validation cohort, and its specificity was 78% in the discovery cohort and 82% in the validation cohort.
The investigators then developed a lipodomic signature to assess the severity of steatosis in NAFLD patients, using magnetic resonance (MR) hepatic fat fraction data as the standard. This lipodomic signature correlated with MR with an r value of 0.81 (P less than .0001).
Next, they evaluated metabolomics for diagnosing nonalcoholic steatohepatitis (NASH). A model that accounted for body mass index (BMI) and the relative concentrations of 20 triglycerides distinguished biopsy-confirmed nonalcoholic fatty liver without steatosis from NASH with an AUROC of 0.95, a sensitivity of 0.83, and a specificity of 0.94 in the discovery cohort. In the validation cohort, the AUROC was 0.84, sensitivity was 79%, and specificity was 92%.
Finally, the researchers developed a way to use metabolomics to evaluate the severity of fibrosis. An algorithm that incorporated 16 variables for phospholipids, triacylglycerols, and nonesterified fatty acids distinguished F0 from F1 through F4 fibrosis with an AUROC of 0.92. Its sensitivity was 90%, and its specificity was 77%. A separate algorithm that incorporated five variables for phospholipids, triacylglycerols, acylcarnitines, sphingolipids, and sterols distinguished F1/F2 fibrosis from F3/F4 fibrosis with an AUROC of 0.89. Its sensitivity was only 62%, but its specificity was 93%.
This proof-of-concept study supports the idea that NAFLD and NASH cause metabolic changes, which in turn alter the circulating metabolome and can be noninvasively measured for diagnostic purposes, Dr. Puri concluded.
Dr. Puri did not list funding sources. He reported having no relevant financial conflicts of interest.