AT THE ADA SCIENTIFIC SESSIONS
NEW ORLEANS (FRONTLINE MEDICAL NEWS) – For many patients with type 1 diabetes mellitus, crossing multiple time zones by airplane upset their disease self-management. In fact, results from a new survey found that 74% reported more hyperglycemia and/or hypoglycemia while traveling overseas, and 9% avoided international travel altogether because of their disease.
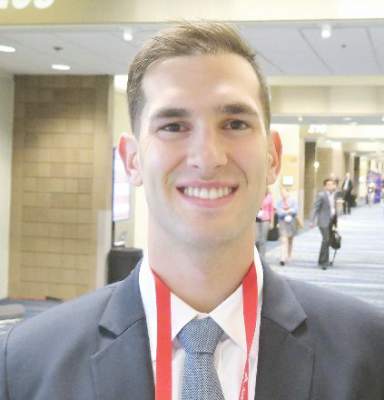
“Travel has become a ubiquitous feature of modern day life. Every day around the world approximately 8 million people board an aircraft,” Benjamen E. Schoenberg said at the annual scientific sessions of the American Diabetes Association. “Based on known rates of diabetes and how often people travel, the Centers for Disease Control and Prevention and the U.S. Travel Association estimate that annually in the United States alone approximately 17 million individuals with diabetes travel for leisure, and approximately 5.6 million travel for business, and these numbers are rising by the year.”
Noting limited existing medical literature on the topic, Mr. Schoenberg of the William Sansum Diabetes Center, Santa Barbara, Calif., and his associates set out to examine the real-life experiences of individuals with type 1 diabetes traveling long-haul by airplane – defined as crossing multiple time zones. They invited members of an online community of the T1D Exchange known as Glu to complete a 45-question online survey that collected information on respondents’ diabetes history, use of technology in self-management of their diabetes, and overall travel experiences.
Of the 503 survey respondents, 71% were female, their average age was 44 years, and 75% had type 1 diabetes for longer than 10 years. The majority of respondents (81%) reported currently having a passport, and 71% reported flying long-haul at least once in the past 5 years. Nearly three-quarters of respondents (74%) experienced increased levels of hyperglycemia and/or hypoglycemia while traveling overseas, 22% ran out of insulin at some point during a trip in the past 5 years, and 9% reported avoiding international travel altogether because of problems related to diabetes management.
Mr. Schoenberg, who is an incoming first-year medical student at Thomas Jefferson University, Philadelphia, went on to report that about one in three participants indicated that their insulin “does not work the same” in flight, compared with when they’re not flying. At the same time, 5% believe that their continuous glucose monitors are less reliable in flight, and about 10% believe that their insulin pumps are less reliable in flight.
When asked what practical difficulties they faced while traveling with type 1 diabetes, the top three responses from survey participants were airport security, taking enough supplies, and crossing time zones. “Furthermore, we found that pump users experienced more difficulty with airport security than non–pump users; 42% of pump users wore their device through body scanners, and 44% reported having at least one negative experience with airport security in the past,” he said.
When asked about their greatest fear of flying long-haul, the top four responses were more hyperglycemia and/or hypoglycemia, problems with airport security, losing supplies, and glucose variability. In addition, only about 30% of respondents reported being satisfied with currently available resources intended to help people manage their disease while traveling. “There is a call to action for providers and nonprofits to continue to develop information to better suit the needs of individuals traveling with [type 1 diabetes],” Mr. Schoenberg said. “Furthermore, 55% reported that they use the Internet as their primary source and about one in four use a smart phone regularly for their self-management.”
He concluded that long-haul air travel with type 1 diabetes “is neither straightforward nor easy. Real-life experiences suggest an unmet need for personalized information. There also may be a need to evaluate insulin and devices at altitude and across time zones. Finally, the impacts of long-haul travel become more relevant as we move toward a commercial artificial pancreas system.” The researchers reported having no financial conflicts.