FROM ACC 17
The small interfering RNA molecule inclisiran has achieved significant reductions in LDL-cholesterol levels in patients at high cardiovascular risk, according to data presented at the annual meeting of the American College of Cardiology and published simultaneously in the New England Journal of Medicine.
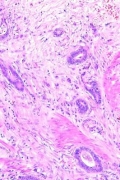
Inclisiran is an investigational, chemically synthesized, small interfering RNA molecule that targets the liver-derived serine protease proprotein convertase subtilisin-kexin type 9 (PCSK9), which promotes degradation of the LDL-receptor.
An earlier phase I trial of inclisiran in healthy volunteers showed sustained reductions in LDL-C levels. In this phase II randomized, placebo-controlled trial, researchers tested a single dose (200, 300, or 500 mg) or double dose (100, 200, or 300 mg on day 1 and day 90) subcutaneous injection, compared with placebo in 501 patients with elevated LDL-C who were at high risk for cardiovascular disease.
By day 30 after the first injection, mean reductions in LDL-C ranged from 44.5% to 50.5% below baseline levels across all dosages of inclisiran (N Engl J Med. 2017 Mar 17. doi: 10.1056/NEJMoa1615758).
By day 180, the mean reductions in LDL-C were 27.9%-41.9% in patients who received a single dose and 35.5%-52.6% in those who received a double dose. By comparison, patients who received placebo showed a 2.1% mean increase in LDL-C.
All patients who received two 300-mg doses of inclisiran showed reductions in LDL-C by day 180, with a mean absolute change of –64.2 ± 20.7 mg/dL. More than half of this group (54%) achieved LDL-C reductions of 50% or more below baseline.
In this same dosage group, 5% of patients achieved LDL-C levels below 25 mg/dL, 48% achieved levels below 50 mg/dL, and 66% achieved levels below 70 mg/dL by day 180 after the first dose.
Researchers observed a nadir in patients’ response at around day 60 for the single-dose group and day 140 for the double-dose group.
“Maintaining consistent and effective reductions in LDL-cholesterol levels in the long term through the use of statins is, in part, hindered by adherence,” wrote Kausik K. Ray, MD, of Imperial College London, and his coauthors. “Hence, approaches that not only lower LDL-cholesterol levels safely but also can maintain reduction consistently over time, when applied either in lieu of or simultaneously with statin therapy, are being sought.”
However, they also clarified that it was still unknown as to whether these LDL-C reductions would translate into reductions in cardiovascular events.
Researchers also saw significant declines in PCSK9 levels from baseline in all patients who received inclisiran. Among those who received a single dose, mean reductions in PCSK9 at 180 days ranged from 47.9% to 59.3%, while those who received a double dose showed mean reductions ranging from 53.2% to 69.1%.
The overall rate of adverse events was similar between the inclisiran and placebo groups (76% vs. 79%, respectively), while the rate of serious adverse events was 11% in the inclisiran group and 8% in the placebo group.
One patient in the inclisiran group and one in the placebo group showed increased levels of hepatic aspartate aminotransferase, and three patients in the inclisiran group had elevated alanine aminotransferase. No increases in bilirubin levels were observed.
“Symptoms of immune activation, which is often a concern with therapies targeting RNA, were rare in association with inclisiran: There were few instances of flu-like symptoms and no observed elevations in C-reactive protein,” the authors wrote.
Injection-site reactions were also relatively uncommon, occurring in 4% of patients treated with one dose of inclisiran, 7% of those treated with two doses, and none of the placebo group.
The authors, however, said that, given the small size and relatively short duration of the trial, they could not rule out the possibility of other infrequent serious side effects. A long-term open-label study also is being conducted.
The study was funded by the Medicines Company. Several authors declared receiving personal fees from pharmaceutical companies outside the submitted work and 10 also declared receiving personal fees from the Medicines Company, 6 involving the submitted work. One author was an employee of the Medicines Company with stock options.