Patient Pages: Data Privacy from Patient Perspective
 Now that many of today’s innovations are data driven, a lot of conversation is centered around regulating patient data: who can get it and how it should be used. PulsePoint conducted a survey of 1,000 patients to see where consumers draw the line with data privacy and how the life sciences industry should respond. Importantly, the top three risks patients associate with sharing their health data are 1) discrimination: insurance companies will use data to discriminate (50%) or employers may use health data to keep people in certain categories from jobs (35%); 2) security: meaning even privately shared data is accessible (41%); and 3) exploitation: health data will inevitably be used for commercial purposes (31%).
Now that many of today’s innovations are data driven, a lot of conversation is centered around regulating patient data: who can get it and how it should be used. PulsePoint conducted a survey of 1,000 patients to see where consumers draw the line with data privacy and how the life sciences industry should respond. Importantly, the top three risks patients associate with sharing their health data are 1) discrimination: insurance companies will use data to discriminate (50%) or employers may use health data to keep people in certain categories from jobs (35%); 2) security: meaning even privately shared data is accessible (41%); and 3) exploitation: health data will inevitably be used for commercial purposes (31%).
PulsePoint found that many patients (64%) want to receive targeted, relevant information about healthcare products without having to see a doctor, but many (51%) don’t want that targeting to come from their search history or clicks. Marketers should note that 54% of these patients are OK with behavioral marketing once they’ve been assured that their data is not being stored.
Patients do want their information to be stored and shared in very few situations, such as those who may be close to life-or-death situations. When patients surveyed were presented with two dangerous scenarios in particular, they supported data sharing. Seventy-nine percent said they support a patient’s EHR sharing information with their doctor about prescriptions that could have dangerous interactions with each other and 75% support their data being shared if they were brought to an ER unconscious and access to their medical records prevented the ER doc from making a dangerous decision.
Besides digital privacy, many of the patients PulsePoint surveyed were hesitant about new technologies such as artificial intelligence and genetic information sharing. Sixty-two percent are in favor of using their genetic data to get a more complete diagnosis and treatment plan from what had been understood to be a limited genetic test around a pregnancy.
PulsePoint also found out how patients feel about trading data for financial incentives. About half of the respondents would share their information with insurance companies for straight discounts, but only 39% would be willing to take on required behaviors based on data shared, even understanding that these behaviors are intended to improve their health, in order to receive discounts. While harvesting data might be done with financial rewards, controlling behaviors to collect outcome data is much less feasible.
Med Device Department: Digital X-rays Are Here
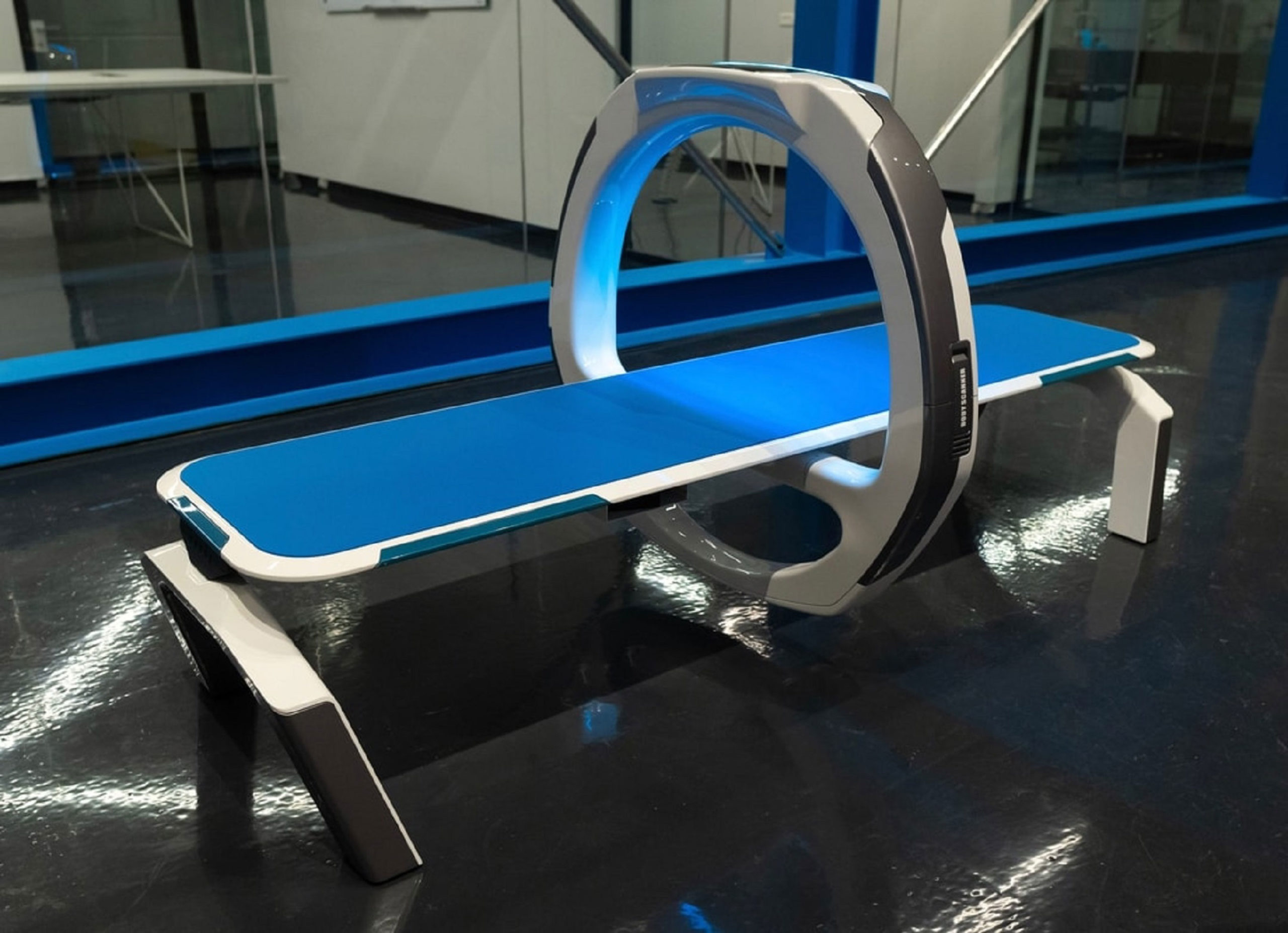
Israeli startup Nanox believed it was time for the traditional X-ray to get an upgrade. The FDA agreed, approving their first product—the Nanox.ARC, a new kind of X-ray machine. The Nanox.ARC machines are light and compact, fitting in doctor’s offices more easily, but more importantly, they emit much less radiation than traditional X-ray machines at a fraction of their price.
The Nanox.ARC is powered by proprietary silicone chips that line the moving ring mounted on the patient table. These chips are stuffed with 100 million nanocones that emit X-rays with pulsating beams as opposed to the continuous radiation of traditional X-ray machines. Having achieved clearance for their single-source product, Nanox hopes to get quick clearance for multisource Nanox.ARC and the accompanying software, Nanox.CLOUD. With this, they will deploy the entire commercial imaging system across the globe in an attempt to make X-ray imaging much more accessible.
“We believe we are well-positioned to achieve our goal of democratizing medical imaging and expanding the market to the roughly two-thirds of the world’s population who currently have limited or no meaningful access to imaging or the preventative screening that it offers,” CEO and Chairman Ran Poliakine stated on the Nanox website. Currently, an X-ray session costs about $300, but this more affordable technology would slash that price.
Therapeutic Talk: Coronavirus and the Nervous System
By now, it is well known that the COVID-19 virus can attack the nervous system of some individuals, causing effects we have yet to fully understand. Researchers at the Institut national de la recherche scientifique (INRS) in Quebec are already working on ways to prevent the virus from spreading to the nervous system. They are the first to find an antiviral immunity from the production of interferons, which detect the early presence of the virus and modulate cleavage of other S proteins.
Marc Desforges, a Medical Biologist specialist at CHU-Sainte-Justine virology laboratory, explains that cleaving S protein by various cellular proteases (such as interferon) is what allows coronaviruses to effectively infect cells and spread to various organs and systems in the body, including the central nervous system (CNS). Therefore, interferon, produced by the olfactory receptors and cerebrospinal fluid in our own brains, can modulate S protein cleavage and significantly reduce the virus’ ability to infect the CNS.
Lead scientist of the study at INRS, Dr. Pierre Talbot, said in a statement, “Using a common cold coronavirus, similar to SARS-CoV-2, we were able to show that cleavage of the S protein and interferon could prevent its spread to the brain and spinal cord in mice.” These promising results tell us that there are two potential targets for CNS antiviral protection: S protein cleavage and interferon production. This creates more opportunities for effective therapies.
Trend Setting: Antibody Development Revolution
Antibody treatments have become a buzzword ever since we heard that COVID-19 antibodies provided possible immunity to the virus. However, those with chronic conditions such as cancer, Crohn’s disease, or psoriasis have been vying on antibody injections as an effective form of treatment for years. The problem is, antibody production is costly and time-consuming, making them inaccessible to most patients.
Efforts to drive down antibody production costs may have finally paid off. Andrew Zydney, Chair and Chemical Engineering Professor at Penn State, has identified a new method of production known as precipitation. Precipitation has been used to process blood plasma for more than 70 years, but has never been applied to antibody production. The process requires adding zinc chloride and polyethylene glycol to a solution containing the antibody. This causes the antibody to precipitate so that the impurities can be washed away. Currently, antibodies are processed using Protein A immobilized in a chromatography column. However, a single Protein A chromatography column can cost more than $10 million.
“That is just one step in the current manufacturing process, and it is what makes antibody manufacturing so expensive,” Zydney told Penn State News. “All of the major biotechnology companies are big players in this space.” He explains that the zinc chloride necessary for precipitation is a simple, cheap salt that can yield large quantities in a shorter amount of time. He believes eliminating the expensive step is the key to enabling biopharmaceutical companies to produce lower-cost antibodies for the patients who need them.
FDA Update
Drug Approvals
Abecma, a idecabtagene vicleucel therapy by Bristol Myers Squibb, received FDA approval for treating adult patients with multiple myeloma who have received four or more prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody. The CAR T-cell therapy requires using a patient’s own T-cells, genetically modifying them and reinjecting them back into the body. This is the first approved gene therapy for multiple myeloma.
Merck’s Keytruda was approved for another indication and can now be used with platinum and fluoropyrimidine-based chemotherapy for patients with metastatic or locally advanced esophageal or gastroesophageal (GEJ) carcinoma.
The FDA granted accelerated approval to TG Therapeutics’ Ukoniq, a kinase inhibitor meant to treat either relapsed or refractory marginal zone lymphoma (MZL) after one prior line of therapy or relapsed or refractory follicular lymphoma (FL) after three prior therapies. The kinase inhibitor includes PI3K-delta and casein kinase CK1-epsilon, which is taken once a day orally for as long as needed.