As physicians look for ways to help them deal with the COVID-19 pandemic, Doximity, the largest community of healthcare professionals in the country, has experienced a surge in activity for many of its offerings. Much of that surge has been for the use of its Doximity Dialer, with the number of calls made by physicians through the app averaging one million per day—which is 20x more than before the pandemic.
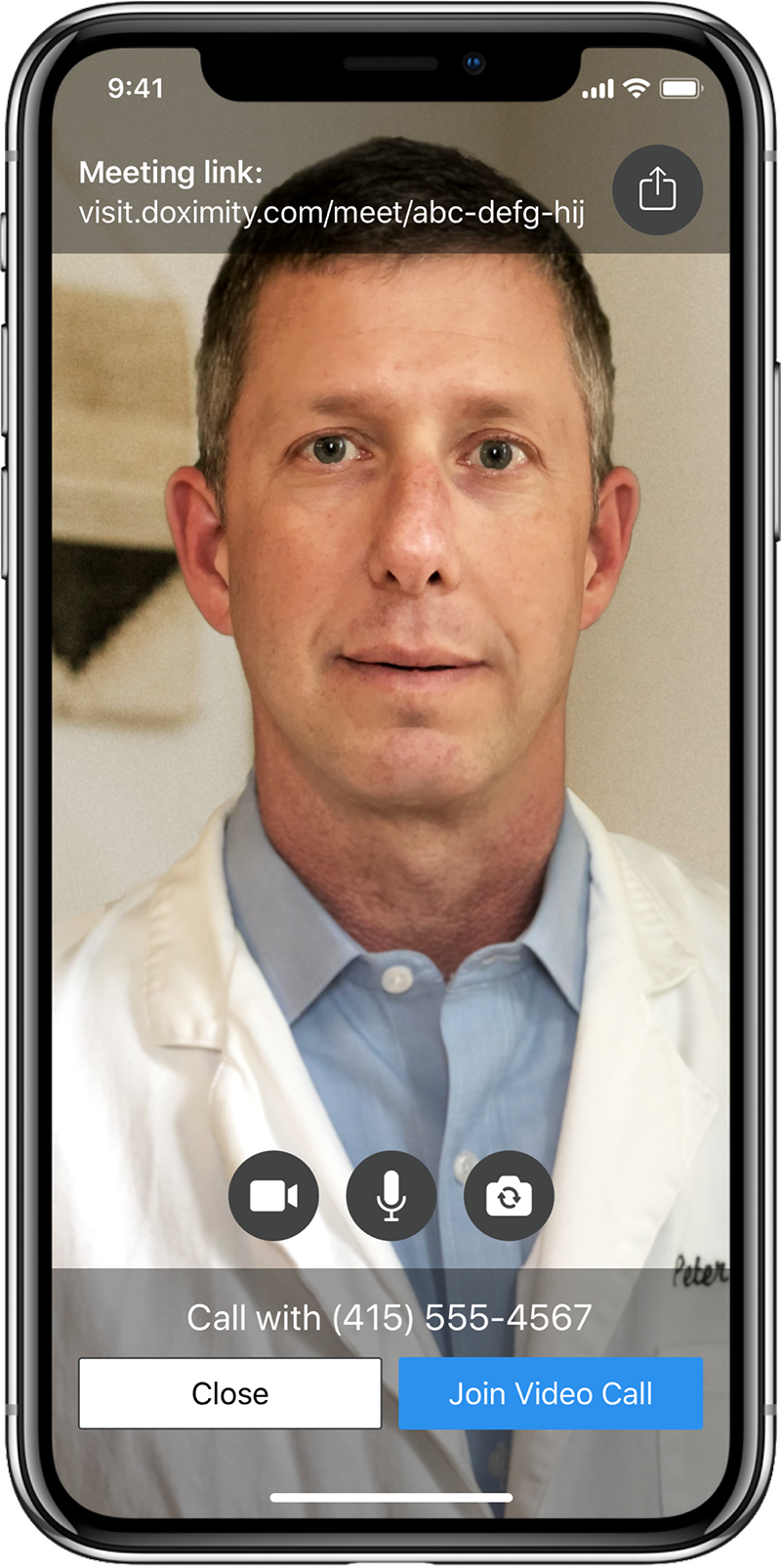
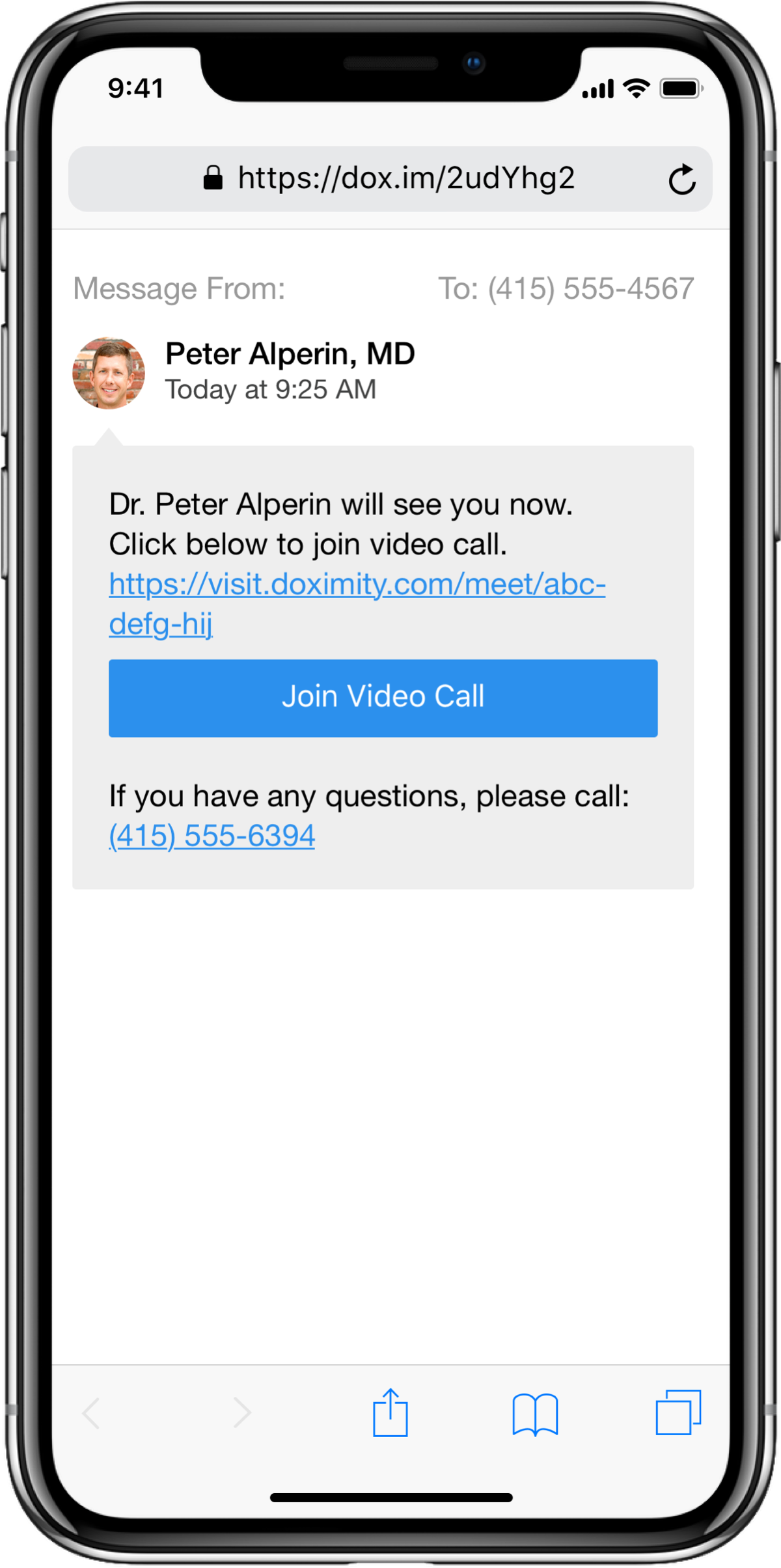
Doximity Dialer allows physicians to securely call patients from their cell phones while masking the call by having it appear as the physician’s office number on a patient’s Caller ID. But due to a high-level of requests for a telemedicine offering, Doximity has launched a new functionality within its app—Doximity Dialer Video. This allows physicians to now make secure videos calls with patients.
 PM360 spoke with Dr. Amit Phull, Medical Director at Doximity, about how the company is handling this surge in activity, its new Doximity Video offering, how the healthcare system needs to change to better handle the pandemic, and what personally concerns him the most as a practicing physician.
PM360 spoke with Dr. Amit Phull, Medical Director at Doximity, about how the company is handling this surge in activity, its new Doximity Video offering, how the healthcare system needs to change to better handle the pandemic, and what personally concerns him the most as a practicing physician.
PM360: What has Doximity done to better handle this surge of activity you have seen and better address physicians’ needs at this time?
Dr. Amit Phull: Due to the surge in activity, we expanded the concept of accessibility to some of our tools and resources to physician’s care team. Many physicians are relaying a lot more on ancillary staff to expand their footprint as they’re being spread more thinly across an increased patient population that in certain parts of the country has surged to the point of overwhelming the system. So we expanded access to Doximity Dialer to folks who are physician extenders, such as NPs, PAs, nurses, clinical psychologists, research coordinators, etc.
Additionally, we spun up a COVID-19 newsroom. One of the issues I ran into myself in my own practice, as well as strong feedback we received from users across the network, was that there was so much information and often misinformation out there that it was even hard to keep track of the core science. So this resource center aggregates up-to-date guidelines, stories from the front line, news as to the evolving science and research, etc. And we made it sticky on the news feed so folks can navigate back into the Doximity news feed and relatively easily stay up to date on vetted COVID-19-related information.
Lastly, we expanded our careers business to provide as a service to many of the health systems in need of workers by giving them the ability to post jobs for free as well as search for physicians. For instance, physicians who have volunteered to serve in hot spots can actually leverage the postings on the Doximity network to facilitate the exchange of that information.
Did you develop Doximity Dialer Video specifically due to COVID-19?
While we had been working on this before COVID-19, this was really the kick in the pants that got us to release this to our users more quickly than we otherwise would have. We were getting a lot of requests from physicians on the front lines that they would love to be able to leverage this software to have telemedicine visits with their patients.
I know from my own experience in the emergency department that folks were using video technology just to speak with patients from the other side of the door as an infection control measure, so we knew how much doctors needed more telemedicine offerings. We didn’t want our platform to be onerous either on the physician user or on the patient, so it doesn’t require patients to download an app. Physicians can use the platform to send a quick text to a patient and then they will meet you in a virtual room where you can then conduct your telemedicine visit.
 Since physicians were requesting that functionality from you, are you seeing or hearing anything else from physicians at this time about what other services or information may benefit them as they deal with the pandemic?
Since physicians were requesting that functionality from you, are you seeing or hearing anything else from physicians at this time about what other services or information may benefit them as they deal with the pandemic?
At a high level, it’s a reemphasis of many of the focuses that we’ve had in our services and offerings throughout or even in the times before the pandemic hit. For example, a big one is being able to access things at the point of care more easily on the communications front.
I think that even breaks down into two component parts where you have folks in a variety of specialties, emergency medicine, critical care, internal medicine in some instances that are “on the front lines.” But this pandemic and what it’s done to the healthcare system has also had pretty significant ramifications for folks across specialties. So being able to filter into that type of content and present it in an organized or easily accessible fashion to all specialties across medicine so that they can be up to date as to what is impacting their practice and their patient population. And frankly, it is also about continuing to provide the specialty-relevant information that was already pertinent. One of the crises hidden within COVID-19 is the fact that it’s complicated patients’ abilities to see their physicians for their chronic conditions that still necessitate care.
Additionally, physicians want to be able to communicate with other verified physicians and share information. That was communicated to us by folks on the front line at the outset of this pandemic. They were having difficulty actually sharing their experiences with others. A lot of physicians and health systems were caught quite flat footed when this hit, and medical journals don’t operate at a rapid enough pace to absorb what is happening and then distribute the type of information fast enough to influence practices. So, the ability for physicians to connect with one another on the Doximity network became a pretty vital resource for folks to be able to exchange information so that they could adopt new practice approaches in real time as the state of affairs on the ground changed hour to hour.
You mentioned healthcare institutions were caught flat footed when the pandemic really hit here in the U.S. Do you see health systems and practices making changes to how they practice medicine now going forward because of this?
We actually worked with researchers from Harvard Medical School and launched a survey to get U.S. physician input across all specialties as to how what was going on was changing their practice, whether or not they felt they themselves were safe, and if their health system or the government was prepared for this.
There were about 2,600 total respondents. Of those, 80% responded they’re moving to or already have transitioned to a much larger proportion of their practice being virtual or employing technologies of telemedicine. So I think that’s a trend that had already begun to show some signs of growing, but with this pandemic it’s certainly here to stay.
The light has also been shown again on the idea of physician dissemination of information. As I mentioned earlier, your typical peer review journal process is not the best machine to fuel the need for up-to-date information and even just dissemination of things such as guidelines and practice patterns in this kind of environment. Even prior to this pandemic, certainly over the course of the last five to 10 years, there was this evolving digital divide that existed in healthcare where the way that knowledge was generated and then communicated across the entire industry contained some choke points that created this large gap physicians had to fill by seeking out their own sources of vetted information.
I think this pandemic has placed a huge strain on that system and identified how physicians communicating with one another and really communicating their experience on the front lines is a route through which you can actually collaborate and get the information you need faster. So I think learning through platforms will have a pretty significant staying power after this.
Since you’re still a practicing physician, have you done anything in terms of working in hospitals and dealing with COVID patients?
I’m an ER physician and I work in Northwestern in Chicago. I was out there a little bit ago. Our situation in Chicago is certainly picking up and the I think the way that all of us have been watching models across the country, Chicago is a little bit delayed compared to the New York area as well as New Orleans and a couple other of the hot spots. I’m also part of the medical reserve corps in New York City and essentially waiting assignment there if there’s need in the short term. So it’s a point of personal concern for what the fall looks like because I think if we don’t change some things in healthcare systems at large then come fall it could be as problematic if not even a greater problem than what we just lived through.
So then what changes do you think healthcare systems still need to make?
Better communication with patients and leveraging existing technologies more aggressively is something that can be employed at the level of the individual physician as well as from a system perspective. And it almost sounds foolish to say it out loud, but we need to focus on preparedness.
I think the healthcare industry has suffered from many of the things that almost any other industry has where there’s just been an extreme focus on supply chains that are ultra-efficient and are as lean as possible. That is great from the perspective of operating a business, but it’s not so great in terms of the robustness that we have at our disposal to respond to these types of once in a hundred year like scenarios. I’m hoping at the health system level we can collectively come out of this having learned that lesson, even if it is the hard way.
All right, is there anything else you would like to add about the pandemic or what needs to be done?
I always add this when I chat with people about this, there’s been this ease based on how people and governments are beginning to take their foot off the gas somewhat. As a provider, that is what gives me the most pause. Circling back to that survey we ran, we asked physicians as to whether or not they thought stay-in-place orders were sufficient. And the majority of physicians thought that they were the right thing to do but may not be sufficient. So I myself, as well as many of the physicians that I interact with, are concerned about easing off maybe a little bit too aggressively and what those ramifications might be on this infection not going away and on the overall psyche of people as we have to deal with a longer-time horizon of this new normal. We take that into account in terms of how we’re approaching building technology at Doximity, just to make sure that we have that flexibility to rise to the occasion regardless of where it takes us.