FROM NATURE
Versions of the complement component 4 (C4) gene demonstrated distinct relationships with schizophrenia risk, with the strongest association linked to a variation that increased expression of C4A, results from a novel study showed.
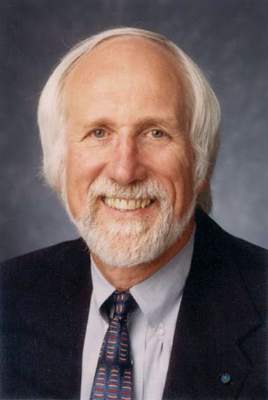
“Although treatments exist for the psychotic symptoms of schizophrenia, there is no mechanistic understanding of, nor effective therapies to prevent or treat, the cognitive impairments and deficit symptoms of schizophrenia, which are the earliest and most constant features of the disorder,” researchers led by Steven A. McCarroll, Ph.D., wrote online in Nature. “An important goal in human genetics is to find the biological processes that underlie such disorders.”
In a study funded by the National Institutes of Health, Dr. McCarroll of the Broad Institute, Cambridge, Mass., and Harvard Medical School, Boston, and his associates analyzed the genomes of 65,000 people, 700 postmortem brains, and mouse genetic engineering to link specific gene versions of C4 (C4A and C4B) to a biological process that could be responsible for at least some cases of schizophrenia. The discovery came about when the team began to search for “cryptic genetic influences that might generate unconventional genetic signals.” They focused on C4 in part because of the association between the protein-coding gene CSMD1 and schizophrenia, which encodes a regulator of C4. They found that the more a version resulted in expression of C4A, the more it was associated with schizophrenia (Nature. 2016 Jan 27. doi: 10.1038/nature16549).
“The more a person had the suspect versions, the more C4 switched on and the higher their risk of developing schizophrenia,” according to a written statement generated by the NIH announcing the work. “Moreover, in the human brain, the C4 protein turned out to be most prevalent in the cellular machinery that supports connections between neurons.”
After adapting mouse molecular genetics techniques as a way to study synaptic pruning and C4’s role in immune function, the researchers also discovered that C4 promoted synapse elimination, or “pruning,” during the developmentally timed maturation of a neuronal circuit. The overall findings “could help explain schizophrenia’s delayed age-of-onset of symptoms in late adolescence/early adulthood and shrinkage of the brain’s working tissue,” Thomas Lehner, Ph.D., director of the Office of Genomics Research Coordination at the National Institute of Mental Health, said in the NIH statement. “Interventions that put the brakes on this pruning process-gone-awry could prove transformative.”
Dr. William T. Carpenter Jr., professor of psychiatry and pharmacology at the University of Maryland, Baltimore, who was not involved in the study, said in an interview that, if synaptic pruning is an aspect of schizophrenia pathophysiology, it’s “important to think of timing and what aspect of schizophrenia would be relevant. For example, cognition impairment is early, years in advance of psychotic symptoms and diagnosis, and not a good target for explaining late adolescent/early adulthood onset of this aspect. Primary negative symptoms may also be present well in advance of psychosis. For present purposes, hallucinations, delusions and thought disorder may be more likely clinical targets.”
Dr. Carpenter, who is also editor-in-chief of Schizophrenia Bulletin, went on to note that synaptic pruning pathology “could be either too much, too little, or simply suboptimal pruning, leaving connectivity inefficient,” adding that “here, a mechanism for excessive pruning is provided that may be relevant to the observed decrease in neutrophil. Having a mechanism hypothesis advances hypothesis testing research and is a valuable contribution.”
The researchers, including members of the NIMH-funded Schizophrenia Working Group of the Psychiatric Genomics Consortium, concluded their article by noting that the human genome “contains hundreds of other genes with complex, multi-allelic forms of structural variation. It will be important to learn the extent to which such variation contributes to brain diseases and to all human phenotypes.”
The study was funded by the NIH. The authors reported having no financial disclosures.