AT THE ASCRS ANNUAL MEETING
SEATTLE (FRONTLINE MEDICAL NEWS) – As patient satisfaction becomes increasingly important for reimbursements, it might be a good idea to switch to propofol for colonoscopies.
The reason is because patients prefer propofol over standard-of-care fentanyl/midazolam as their anesthetic for outpatient colonoscopies, according to a randomized, blinded trial at a single center. Importantly, clinical assessment also showed that propofol outperformed fentanyl/midazolam in terms of hypoxia, pain, nausea, and procedural difficulties.
The 300 patients randomized to propofol were more likely than were the 300 randomized to fentanyl/midazolam to rate the amount of anesthesia they received as being “just right” (98.7% versus. 91.3%), and they were more likely to state that they were “very satisfied” with their anesthesia during the procedure (86.3% versus 74%). Propofol patients were also more likely to recommend their anesthesia to others (98.7% versus 94%).
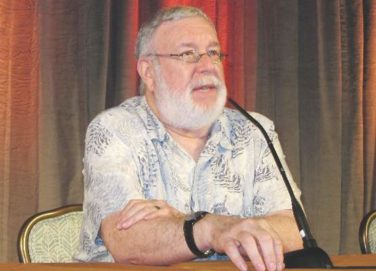
“Our study demonstrated the superiority of propofol over fentanyl/midazolam in an outpatient setting from both a patient satisfaction standpoint and from a provider prospective,” said lead investigator Anantha Padmanabhan, MD, a colorectal surgeon with Mount Carmel Health, Columbus, Ohio.
The short duration of action and quick turnaround time have led to an increase in the use of propofol for outpatient procedures. It’s been studied extensively for safety and efficacy, but patient preference has not been well documented. The investigators wanted to look into the issue because patient satisfaction has become an important metric for reimbursement, Dr. Padmanabhan said at the annual meeting of the American Society of Colon and Rectal Surgeons, where the study was presented.
Patients were randomly assigned to propofol or fentanyl/midazolam in the colonoscopy suite at the Taylor Station Surgical Center in Columbus. Anesthesia personnel administered the assigned anesthetic, and circulating nurses rated the difficulty of the procedure. Patients were surveyed after they came to, and again over the phone at least 24 hours after discharge.
Dr. Padmanabhan performed all the colonoscopies in the study. He could not be completely blinded to the anesthetic used, so did not participate in any data collection.
Fewer propofol patients reported pain greater than zero during the procedure (2% versus 6%); fewer remembered being awake (2% versus 17%); and fewer had complications (2.7% versus 11.7%); 21 patients in the fentanyl/midazolam group had intraoperative hypoxia, versus 1 in the propofol group. Eleven fentanyl/midazolam patients had postprocedure nausea and vomiting, versus one propofol patient.
Nurses rated 26% of fentanyl/midazolam procedures as “difficult,” compared to 4.7% in the propofol group. Mean induction time was 2.1 minutes with propofol and 3.2 minutes with fentanyl/midazolam; mean procedure time was about 13 minutes in both groups. The cecal intubation rate was 100% in both groups, and there were no perforations.
Propofol patients reacted less during the procedure; an audience member wondered if the loss of feedback was a problem for Dr. Padmanabhan.
“We use propofol in a very light sedation, and sometimes we do get feedback, but more importantly we feel the technique of colonoscopy is as much by feel as it is by vision. If you feel that the scope is not going in correctly, you should pull back then try the loop reduction maneuvers,” he said.
The most common indication for colonoscopy was a history of polyps, followed by general colon screening. Patients in both groups were a mean of 61 years old, and about evenly split between the sexes. Body mass index was a mean of 30 kg/m2 in both groups. There were no between-group differences in comorbidities; hypertension and diabetes were the most common.
There was no external funding for the work, and the investigators had no disclosures.