FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery ( 2016;151:1239-48 ), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D. , of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
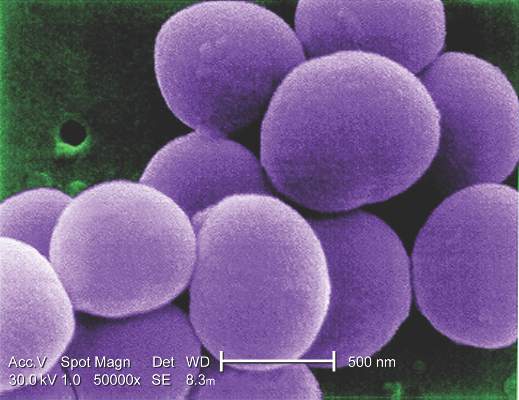
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study ( Ann. Thorac. Surg. 2012;93:480-07 ), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.