When the FDA approved Biogen’s Aduhelm (aducanumab) in early June, it was the first new treatment approved to treat Alzheimer’s disease since 2003. It was also the first-ever treatment directed at the underlying pathophysiology of Alzheimer’s disease, the presence of amyloid beta plaques in the brain, which means the treatment is supposed to reduce the clinical decline that results from this devastating form of dementia.
However, the drug was not approved without controversy. Back in November of 2020, an FDA advisory board comprised of outside experts voted 8 to 1 against recommending approval since Biogen’s late-stage study didn’t provide “strong evidence” that aducanumab effectively treated Alzheimer’s. Two other members of the panel abstained from voting since they thought the data was “uncertain.” Since the approval of Aduhelm was announced, three members of that advisory board have resigned due to the FDA’s decision: Aaron Kesselheim, a Professor of Medicine at Harvard Medical School; Mayo Clinic neurologist Dr. David Knopman; and Washington University neurologist Dr. Joel Perlmutter.
In its statement announcing the approval, Dr. Patrizia Cavazzoni, Director, FDA Center for Drug Evaluation and Research, wrote:
“The data included in the applicant’s submission were highly complex and left residual uncertainties regarding clinical benefit. There has been considerable public debate on whether Aduhelm should be approved. As is often the case when it comes to interpreting scientific data, the expert community has offered differing perspectives.
At the end of the day, we followed our usual course of action when making regulatory decisions in situations where the data are not straightforward. We examined the clinical trial findings with a fine-tooth comb, we solicited input from the Peripheral and Central Nervous System Drugs Advisory Committee, we listened to the perspectives of the patient community, and we reviewed all relevant data. We ultimately decided to use the Accelerated Approval pathway—a pathway intended to provide earlier access to potentially valuable therapies for patients with serious diseases where there is an unmet need, and where there is an expectation of clinical benefit despite some residual uncertainty regarding that benefit.”
Under the Accelerated Approval pathway, Biogen is required to conduct post-approval studies to verify the anticipated clinical benefit. If the confirmatory trial does not verify the drug’s anticipated clinical benefit, the FDA has regulatory procedures in place that could lead to removing the drug from the market.
However, even some of the drug’s supporters were upset once the yearly price of $56,000 was announced. The Alzheimer’s Association, which was a leading advocate for Aduhelm’s approval, said in a statement: “This price is simply unacceptable. For many, this price will pose an insurmountable barrier to access, it complicates and jeopardizes sustainable access to this treatment, and may further deepen issues of health equity. We call on Biogen to change this price.”
Despite all of this controversy, if Aduhelm proves effective it can be a significant breakthrough in the treatment of Alzheimer’s. To get more information on the clinical data and the potential benefit of the medicine, PM360 spoke with Dr. Douglas Scharre, a neurologist and director of the division of Cognitive Neurology at Ohio State Wexner Medical Center. Dr. Scharre has been doing clinical research and trials in Alzheimer’s disease for about 28 years and Ohio State was one of many sites across the world that participated in aducanumab trials.
PM360: Since you have been involved in Alzheimer’s research for so long, I am sure you have seen several potential treatments come and go. In the past, many Alzheimer’s treatments would get to Phase 3, but then fail to show the proper effectiveness to earn approval. Since this is the first approval in almost two decades, what makes this treatment different in your mind in terms of how it works or just how effective it’s been?
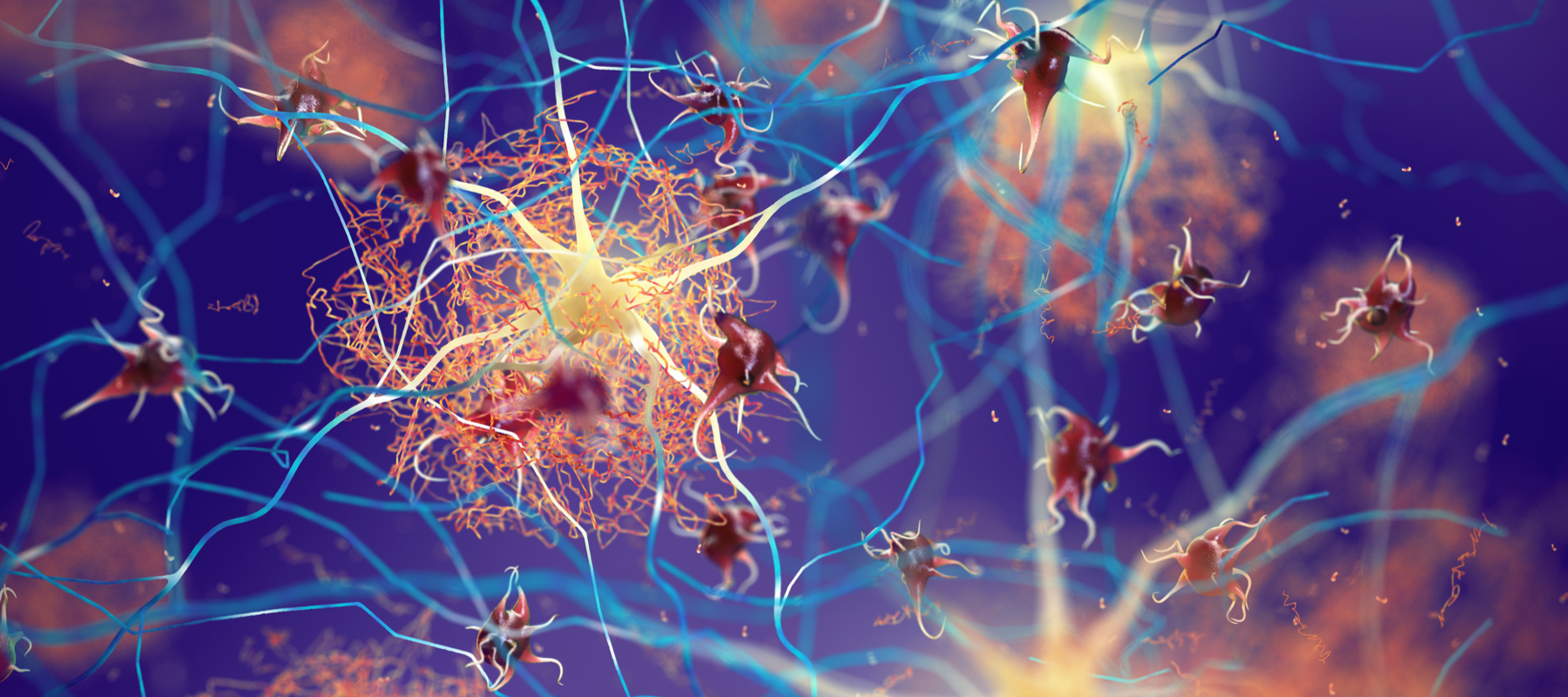
Dr. Douglas Scharre: Well, we’ve had many potential treatments, and many clinical scientists like myself have been working on this problem of Alzheimer’s for a long time. It’s a complex disease, and the brain is complex, so it’s not a simple puzzle to solve. I think there’s multiple cascading events that are occurring that cause the symptoms of Alzheimer’s. You have the amyloid, which is a protein that builds up in the brain and misfolds, accumulates, and is toxic and starts killing nerve cells. You also have a tau protein, which can serve as another trigger for all these other downstream events.
The reason this is exciting to me is that it’s the first disease-modifying agent that we’ve had that was shown to effectively get rid of amyloid. And even though it’s not a cure, it can help a very small sliver of individuals slow their decline, so it’s really a nice first baby step to actually take care of the amyloid. Now we need to work on reducing the tau or reducing inflammation. And I believe in a few years we’ll have five or six treatments at different stages of the disease that are all designed to impact or mitigate the effects of these different pathways that are leading to the symptoms of Alzheimer’s.
In your time investigating different drugs for Alzheimer’s, is this the first one that took this approach? Was there anything specific that led to this breakthrough or approval?
Well, definitely not. We’ve been looking at these antibodies against amyloid for many, many years. Since it was such a key factor in Alzheimer’s, it was an obvious target. So most of the earlier studies seemed to target people with mild to moderate Alzheimer’s dementia. And what we found was that it was just too late and you instead need to target this amyloid protein a little earlier since it’s one of the key initiators of all these downstream different events that are going on because of Alzheimer’s. So, it’s pretty clear that the earlier you start treating Alzheimer’s symptoms, such as very mild cognitive impairment, then you will be much more successful at preventing the disease from triggering all these other pathways that are doing their own damage to the brain.
This approval came with a bit of controversy. As you know, the FDA’s advisory committee originally voted not to move forward with approval and some other groups have expressed concern about the clinical data as well. What do you make of some of these concerns?
I think many of them are very valid. As I said, this treatment would be only useful for people that are in very mild stages of Alzheimer’s. If you’re more in the mild-to-moderate range of Alzheimer’s dementia, then it’s not going to be helpful for you. So we need to be very careful at identifying the appropriate patient and not giving it to individuals where it’s not going to help, because that’s just a waste of healthcare dollars.
From my understanding, it sounded like the FDA approved it more so because it was very effective in getting rid of the amyloid from the brain. It does that very well—and that’s what it was made to do. It goes into the brain, gets the amyloid out. And after 52 to 70 weeks, it’s pretty much to normal range. Considering amyloid is a significant trigger for Alzheimer’s symptoms and all these downstream effects, I think that potentially was the reason the FDA decided to go ahead and approve it.
I’ll just add that one other reason I think it was useful they approved it is that this news will promote attention to the fact that there may be agents that can help with Alzheimer’s if patients see their doctors and are identified very early. I’m hoping this motivates individuals who are beginning to see a little change in their cognition to get in to see their doctors. Get identified. Even if it’s not Alzheimer’s, there are lots of other things that cause cognitive issues and it may be possible they can be treated. And if it is an Alzheimer’s process with amyloid, then we now have this drug that can slow down the course and give you more time. How much time? We don’t know that yet because the studies only took place over a year and a half. So it’s hard to say how long the effect of using this might be for patients, but there is a signal there.
Speaking of that awareness, is that just on the patient end? Or is it also on the HCP end in terms of when to screen their patients for cognitive decline? How can those in healthcare and the life sciences help increase awareness around this and get better early detection to make this drug more effective?
It’s a great question. Often it is the family who notices it first. The patient might as well, but they’re also more forgetful and may not tell their doctor. So the family really needs to encourage them to get to their physician and tell them about their issues.
The physician also then should consider screening. There’s something called the “annual wellness visit” at Medicare age in the U.S. It starts at 65 and it’s a wellness visit to check for cancers and risk factors such as weight loss, depression, etc. Part of that is also assessing for cognitive issues, and at 65 about 3% have dementia, so it’s not a small percentage. I would recommend doctors asking, “Have you been noticing any memory issues?” and if the patient says, “Well, yeah, maybe a little bit,” bingo! You give them a screening test.
I’m biased because I developed one of these types of screening tests at Ohio State, so I would recommend my self-administered test called SAGE. Typically, it is easy for primary care doctors to use any self-screener test because they don’t have to take time to do it themselves. However, any type of screening test used to measure cognitive insight would be acceptable. And then every year the patient comes in you could see if there’s any change over time. So those are some of the ways in which people can be more aware and catch some cognitive change early so that they might be eligible for this new disease-modifying agent if it turns out to be Alzheimer’s.
Given that aducanumab received accelerated approval, the drug still has to go through clinical trials while it’s in the real-world setting just to ensure that it is effective. How will those ongoing studies go and what’s going to be necessary to see in terms of results to keep this drug on the market?
We’ll be involved in some of those ongoing studies to measure individuals in the real-world setting. The key is going to be picking the appropriate patient again. If you choose a lot of patients who are moderate-stage Alzheimer’s, it’s not likely you’ll see any significant change. I’m not saying it wouldn’t help at all, but it probably wouldn’t be very effective. Then when you get the results back, it will appear this drug’s not doing anything. But if you’re able to capture these newer patients who are just starting to have symptoms, then I would expect that you would find the same results that we found in the study. And then, hopefully, in the next few years we’re going to get some of these treatments out that are targeting these other downstream effects. And that’s, as I said, when the combination will really have a significant impact on this disease.
Given your experience in this area, what is your view of the future market in terms of treatments? When do you see us finally getting to that point where we actually have multiple Alzheimer’s treatments on the market giving hope to these patients, especially after seeing so many treatments fail in this space in the past?
Every study we’ve done has given us more information. As with most things in life, you have to go through a lot of failures to get your successes, and we’ve learned from each of these failures very well. And that has provided us insight as to what else we can try. Additionally, the fact that we’re not seeing a fabulous result just by targeting amyloid in these studies is also prompting the scientific community to try other targets and that’s when we’ll really see an impact on this disease.
All of these different tracks and targets to mitigate the effects of these different downstream issues that we see with Alzheimer’s disease are going on in parallel, so I’m hopeful. I think that it’s something we will be able to figure out and have a substantial improvement. I’m not saying that it’s going to be a cure or reverse. But if you’re 85 years old and we can slow down that course of Alzheimer’s for the next 10 years, well, that’s pretty good.
We hope to eventually be able to stave it off just like we do with high blood pressure, diabetes, or cholesterol. There’s really not a cure for those diseases either, we just give medications to keep it at bay so it doesn’t cause the impact on the body or the brain. So that’s the plan right now and there’s an excellent chance for us to achieve it. We’re not there yet. Aducanumab is not that agent, but it’s the first disease-modifying treatment we have and it’s nice to see science to be able to achieve one portion of fighting this disease.