FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Adding bezlotoxumab to standard antibiotic treatment of primary or recurrent Clostridium difficile infection reduces recurrences by 38% (10 percentage points), according to a report published in the New England Journal of Medicine.
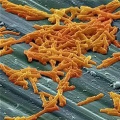
As many as 35% of patients who complete initial antibiotic treatment have at least one recurrence of C. difficile infection, and the rate of repeat recurrence rate jumps to 60% after the initial recurrence. Researchers performed two parallel international phase III trials to assess the efficacy and safety of bezlotoxumab, alone or in combination with actoxumab, for preventing such recurrences. Both monoclonal antibodies work by binding to and neutralizing C. difficile toxins; bezlotoxumab targets toxin B and actoxumab targets toxin A, said Mark H. Wilcox, MD, of the division of microbiology, Leeds (England) General Infirmary, and his associates.
The manufacturer-sponsored trials were randomized, double-blind, placebo-controlled studies involving a total of 2,655 adults (median age, 66 years; range, 18-100 years) treated at 322 medical centers in 30 countries during a 3.5-year period. The study participants received a single 1-hour IV infusion of bezlotoxumab alone, actoxumab alone, bezlotoxumab plus actoxumab, or placebo while taking a standard 14-day oral course of metronidazole, vancomycin, or fidaxomicin. An interim analysis of the trial data showed that actoxumab was not efficacious alone and added nothing to bezlotoxumab treatment, so both study reports focused on the performance of bezlotoxumab.
The primary efficacy endpoint – the proportion of patients with recurrent C. difficile infection during 12 weeks of follow-up – was substantially lower with bezlotoxumab (17%) than with placebo (28%) in the first trial and in the second trial (16% vs. 26%). This treatment benefit was evident as early as 2 weeks after infusion and persisted throughout follow-up, the investigators said (N Engl J Med. 2017 Jan 25. doi: 10.1056/NEJMoa1602615 ).
The agent’s persistent effect through 12 weeks is important to note because approximately 30% of the recurrences in this study “occurred beyond the conventional 4-week assessment period for treatment efficacy. The number needed to treat to prevent one episode of recurrent C. difficile infection was 10; it was 6 among participants 65 years of age or older and those with previous C. difficile infection,” Dr. Wilcox and his associates noted.
Bezlotoxumab was consistently effective in several sensitivity analyses. It also was effective in both trials individually as well as in pooled results. And the choice of oral antibiotic appeared to have no effect on bezlotoxumab’s efficacy.
In a post hoc analysis, bezlotoxumab was also effective in the subgroup of 1,964 patients at highest risk for C. difficile recurrence because they were elderly, had compromised immunity, had the most severe infections, had a history of C. difficile infection, or carried a strain of the organism associated with particularly poor outcomes. In this subgroup, 17% of patients given bezlotoxumab and 16% of those given bezlotoxumab plus actoxumab developed recurrences, compared with 30% of those given placebo.
Regarding adverse events, the agent had “a generally favorable safety profile,” and the rates of adverse events “were generally as expected, given the underlying disease severity, baseline coexisting conditions, and ages of the participants.” Two participants discontinued the infusion because of an adverse event. Drug-related adverse events occurred in 7% of the entire study population, serious drug-related adverse events occurred in 1%, and both occurred at similar rates across the study groups.
Both trials were funded by Merck, which also was involved in study design, data analysis and interpretation, and writing the reports. Dr. Wilcox and his associates reported ties to Merck and numerous other industry sources.
On Twitter @IDPractitioner