With an increasing number of COVID-19 vaccines becoming available, the end of the pandemic is now in sight, but even with efforts to scale up production the supply of vaccines will influence the speed of vaccination. As a result, careful vaccine allocation is needed to maximize social and economic benefits across the U.S. Multiple frameworks have recently been developed to guide vaccine allocation, including one led by our team at CRA and the Center for Global Health Innovation (CGHI) Vaccine Economics and Equity Group (VEEG).1 This new framework offers guidelines for COVID-19 vaccine allocation under conditions of scarcity that considers core public health and ethical principles in the context of optimal benefit to the U.S. economy.
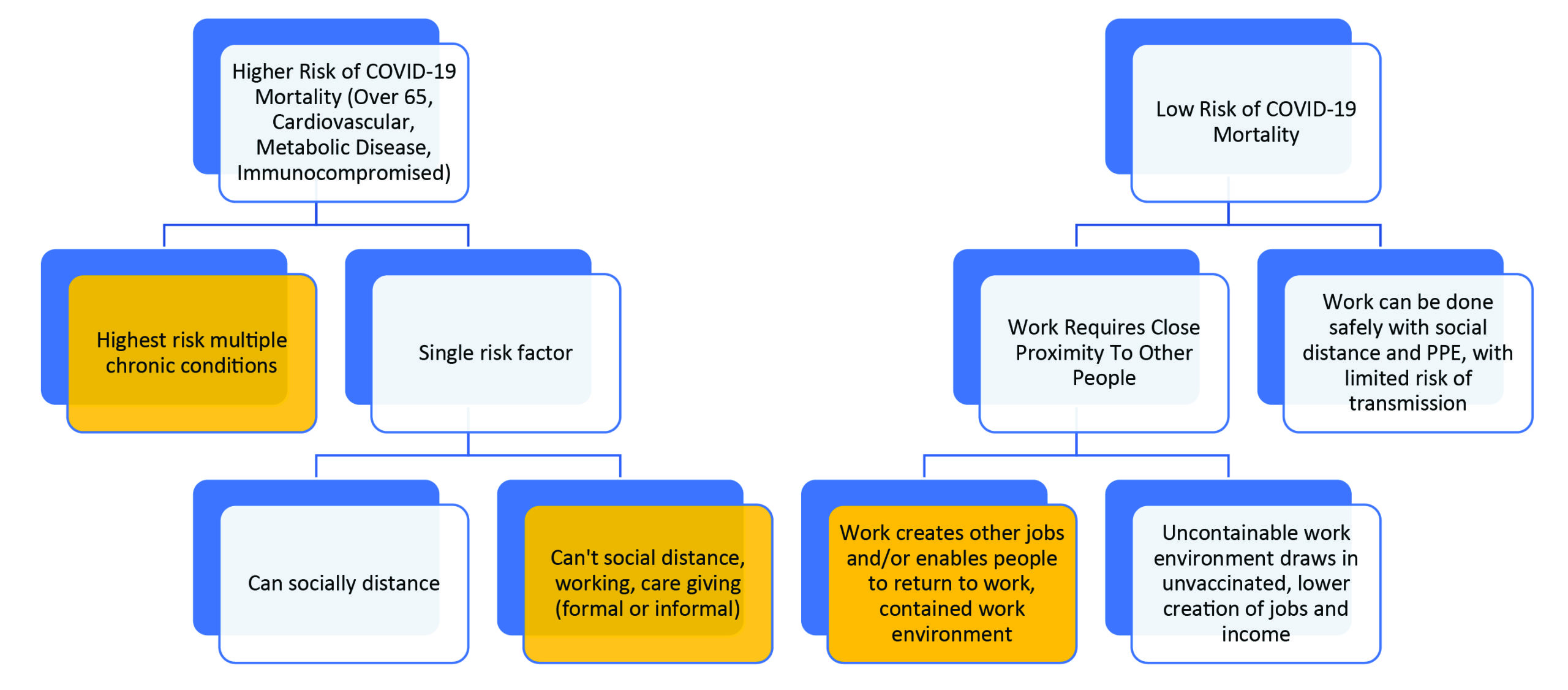
Under this framework, the first objective of ethical vaccine allocation is limiting the harm of the virus to groups at high risk of mortality, including the elderly, people with underlying medical conditions, and front-line care workers. From an economic perspective, protecting healthcare workers can help create other jobs as it facilitates care being provided to others, preserving limited healthcare resources and helping to mitigate the impact of the pandemic.
When vaccine supply is limited, there should be sub-prioritization of healthcare workers based on the amount of time and contact required for patient care and the ability to effectively use personal protective equipment (PPE). For example, home health aides and nurses may be at greater risk than workers who do not have as much daily contact with patients. Social distancing and the use of PPE remain appropriate even with access to an approved vaccine until broad herd immunity is achieved to continue to protect those most at risk of contracting COVID-19.
This framework also seeks to invigorate a stalled U.S. economy. As we have seen in recent months, some jobs can be productively done remotely or with social distancing, while others cannot. A key component of the “reopening prioritization” requires a cost/benefit evaluation of the level of transmission risk based on the nature of work, including:
- if the work relies on proximity to other individuals;
- if a job allows those to work who may otherwise need to be at home (such as caregivers of children or the elderly);
- the value of the industry in creating other jobs (which is often described as an employment multiplier effect); and,
- if the work is instrumental in reducing disease transmission or mortality.
This approach builds on existing allocation frameworks but the criteria for COVID-19 vaccine allocation can be further assessed and refined based on the type of work, the value of the industry to the economy, and the need to be proximate within each industry.
Different Jobs Have Different Economic Value
Economic activity in various industries often has different effects on job creation, both directly and indirectly through a multiplier effect. Industries differ in the job creation generated by their expansion, with respect to supply chain impacts and through purchasing power created by the wages paid. Generally, industries that require costly inputs (such as complex manufacturing) or that are labor-intensive or offer higher wages often have a greater impact on job creation.
When assessing vaccine allocation, you need to trade-off the importance of the industry in job creation and the generation of economic activity with the ability to use social distancing and PPE to control viral transmission. Research shows that much of the work in the two largest U.S. industries (including finance), that account for 34% of gross domestic product (GDP), may be done with social distancing. Work in other large industries that generate significant job growth, such as manufacturing, may not be done remotely and thus workers in these areas should be prioritized for vaccine allocation. It is important to consider that within an industry there may be sub-sectors more amenable to the use of PPE and social distancing and that create more jobs.
Other industries are critical to allowing others to return to work, including education and healthcare. For example, if young children are able to attend elementary school in person then it may allow parents (who may be balancing childcare at home) to work more productively. Parent participation in the workforce is less affected when they have older children in secondary school or college who are often better able to continue their education with social distancing and online learning. Reducing COVID-19 transmission through vaccine allocation for formal and informal providers of young child care and education would likely have a meaningful economic impact and should be a priority to allow others to return to work.
Our framework also recommends several additional vaccine allocation principles to maximize economic implications. These principles emphasize the populations that have been most negatively impacted by the pandemic and cannot work or live productively with social distancing and PPE:
Workplaces Where Immunity Can Be Achieved: Sectors of the economy that bring unvaccinated individuals together should ideally not re-open unless processes are in place to reduce transmission risk (e.g., testing, social distancing, PPE, ability to contact trace). For example, allocating vaccines to industries such as live entertainment and indoor dining would protect workers but has the potential to create harm by gathering those who are not vaccinated. However, those workers should receive sustained financial support to mitigate economic harm.
Prioritization Based on Vaccine Uptake and Data Collection: There is significant variability between states and populations in vaccination rates for influenza2 and other diseases.3 States can elevate vaccination rates through several policies, including providing convenient and trusted avenues for vaccination.4 Collection of data on available vaccines would also help address misinformation, which is a major risk to vaccine uptake. Consideration should be given to creating registries and other data tracking mechanisms, policies to encourage vaccination, and refining the capacity to analyze related health data.
Mitigating the Differential Impact on Low Income and Diverse Communities: Vaccine allocation should also address issues related to income and inequity. Specifically, allocation should consider the greater likelihood of contracting COVID-19 and the probability of related mortality among Black, Hispanic, Native American, and low-income populations.5,6,7 Any vaccine allocation framework should consider the risk of exposure, morbidity, or death, and how that varies among individuals, particularly in the case of COVID-19, which has had a disproportionate impact on certain populations. People who cannot socially distance in their place of work are bearing significant costs, to themselves and the economy, due to the pandemic. Re-starting the stalled U.S. economy will require people to feel confident working, buying goods and services, and interacting socially. These ongoing personal and societal costs need to be considered when allocating approved COVID-19 vaccines.
References:
1. Center for Global Health Innovation and CRA, “Allocating COVID-19 Vaccines With Economic Considerations” https://mk0globalhealthn957w.kinstacdn.com/wp-content/uploads/2020/11/FINAL_CGHI_CRA-Report-Economic-and-Ethical-Framework-for-Vaccine-Allocation-11092020-v2.pdf.
2. CDC. “Estimates of Influenza Vaccination Coverage among Adults—United States, 2017–18 Flu Season.” https://www.cdc.gov/flu/fluvaxview/coverage-1718estimates.htm. Accessed 15 October 2020.
3. CDC. “2008 through 2018 Adult Vaccination Coverage Trend Report.” https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/data-reports/general-population/trend/index.html. Accessed 27 October 2020.
4. Navin, M.C, and Largent, M.A. (2017) “Improving Nonmedical Vaccine Exemption Policies: Three Case Studies,” Public Health Ethics, 10 (3): 225–234, https://doi.org/10.1093/phe/phw047.
5. U.S. Census Bureau, “Current Population Survey, 1968 to 2018 Annual Social and Economic Supplements.” https://www.census.gov/content/dam/Census/library/visualizations/2018/demo/p60-263/figure1.pdf. Accessed 27 October 2020.
6. Ford, T. et al. (2020) “Race Gaps in COVID-19 Deaths Are Even Bigger Than They Appear.” Brookings. https://www.brookings.edu/blog/up-front/2020/06/16/race-gaps-in-covid-19-deaths-are-even-bigger-than-they-appear. Accessed 19 October 2020.
7. CDC. “COVID-19 Hospitalization and Death by Race/Ethnicity.” https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed 19 October 2020.
The views expressed herein are the authors’ and not those of Charles River Associates (CRA) or any of the organizations with which the authors are affiliated.









