To engage leaders of prominent companies and organizations in discussion on today’s critical healthcare issues, the Healthcare Leadership Council (HLC)—a coalition of chief executives from various private-sector disciplines of U.S. healthcare—formed the National Dialogue for Healthcare Innovation (NDHI). Last week’s NDHI summit brought healthcare leaders together in a cross-stakeholder dialogue on value—with a focus on identifying solutions that HLC members could deliver.
In preparation for this summit, ZS—a global consultancy and HLC member organization—interviewed more than 50 HLC members on what constitutes “value” in healthcare and how to better deliver it, innovate and build consensus across the industry.
The aim was to crystallize opportunities to make a positive difference in healthcare, whether through efforts to shape public policy, private-sector collaborations or private-public collaborations.
Defining Value in Healthcare
ZS led the summit presenting the results of its HLC member interviews and attempted to gather consensus on the meaning of value in healthcare. The discussion became nuanced at times as some stakeholders wanted to add qualifiers or other specific terminology to cater the value definition to their respective industries.
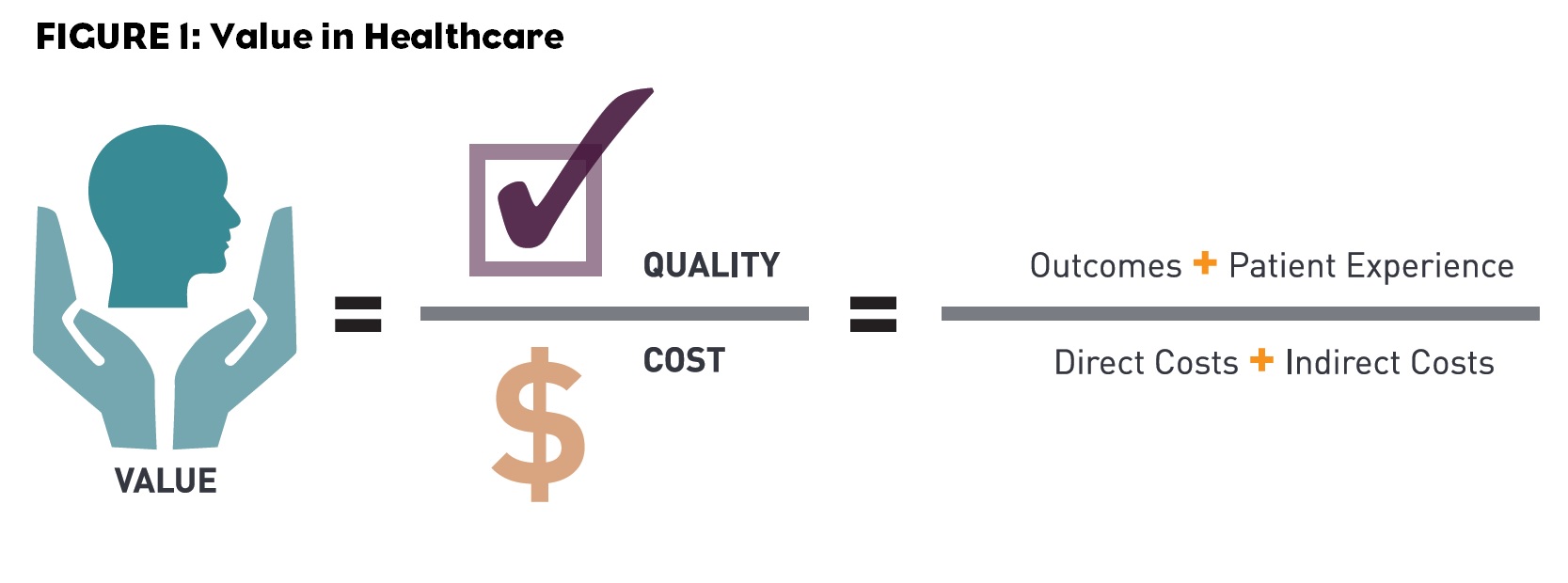
Ultimately, HLC stakeholders generally agreed that “value” in healthcare can be measured as the quality of care provided divided by the total cost of that care (Figure 1). (They noted that the time horizon used to measure value likely varies based on the condition being treated).
Further alignment was generated around the principle that “quality” must take into account not only treatment outcomes, but also the patient’s care delivery experience—though with minimal-to-no focus on what were considered less essential experience drivers, such as parking or hospital food quality.
Barriers to Value Delivery
While HLC members agreed on the overarching value equation, some stakeholders mentioned factors that complicated value delivery. The value of a product or healthcare service is impacted by the time horizon over which its value is determined. Ideally, value should be measured over the lifetime of the patient. In practice, however, measurement is limited to shorter time frames due to various market factors (e.g., patients switch insurers multiple times throughout their lives, publicly traded for-profit organizations that want to appeal to their shareholders and patients are unable to make long-term judgments about their health).
“The short-term nature of the patient-payer relationship is a significant barrier,” observed a health system executive. “How much should payers invest in long-term payback when the patient receiving the benefit will be with another payer down the road?”
Other barriers to value delivery include the misalignment of incentives, trust issues between stakeholders, regulations that discourage collaborations between organizations and a lack of data standardization, interoperability and transparency.
Solutions to Improve Value Delivery
To overcome these barriers, executives described opportunities to collaborate across the healthcare value chain in areas such as payment model pioneer programs, data interoperability standards and value stream mapping by therapy area. Barriers and opportunities discussed in ZS interviews became topics of in-depth conversation at the summit.
During a working session, summit participants discussed barriers to value delivery and collaboration and brainstormed solutions to address them. Many teams discussed barriers outlined in ZS’s report, especially the misalignment of stakeholder incentives.
One representative explained the misalignment from the perspective of the system level compared to the organizational level: Achieving cost savings as a system results in revenue loss for some organizations. Therefore, improving value requires bold private sector pioneers who are willing to engage in downside risk.
The most spirited discussions emerged as summit participants brainstormed opportunities to act as pioneers in healthcare. They rallied around a few specific opportunity areas: Broadening the time horizon of value measurement to encourage innovation, facilitating private-sector collaborations (via regulatory changes or expanded eligibility for anti-kickback waivers) and developing multi-stakeholder medication adherence initiatives.
Developing a Medication Adherence Pilot Program
One of the big hindrances to patient well-being and a source of frustration to providers, payers, pharmacies and pharmaceutical manufacturers is medication adherence. The opportunity to pilot a medication adherence program for one condition (e.g., diabetes, hypertension or congestive heart failure) resonated with the group, especially because the direct cost of non-adherence is approximately $290 billion annually.1
While many have tried to solve the medication adherence issue, a successful, unified program with a multi-stakeholder engagement has not yet been found. Addressing this particular issue is attractive to all stakeholders—there is no “loser” in a successful program. However, other collaboration models that shift risk or change payment models can result in some stakeholders losing out relative to the status quo.
Developing a cross-stakeholder medication adherence program also requires participants to find ways to overcome commonly cited barriers related to building trust, sharing data, aligning incentives and changing behaviors.
All players will likely benefit from an effective program: Pharmacies and manufacturers will sell more medicine; patients and their providers will see better outcomes; payers will avoid medical costs due to non-adherence despite increased drug spend; technology companies will have opportunity to demonstrate how their products can support behavior change.
“A medication adherence pilot would not only impact pharmaceuticals, but also confront many of the broader issues in this discussion: Coordination of care, expansion of midlevel providers, development of patient-centered medical homes, implementation of IT solutions, etc.,” explained one pharmaceutical company executive. “In the end, the pilot brings together and aligns stakeholders in new ways.”
Summit moderator, Ceci Connolly (Managing Director of PwC’s Health Research Institute), provided an inspirational closing statement, urging HLC members to, “think big, start small, and act fast.” HLC can take initial steps in the long journey to improved value in healthcare by promoting the agreed-upon “value” definition and building a multi-stakeholder medication adherence program.
References:
1. http://www.cvshealth.com/2014-insights-report-importance-adherence