BOSTON (FRONTLINE MEDICAL NEWS) – A nonsteroidal anti-inflammatory drug and exercise may be enough to control active axial spondyloarthritis in some patients, suggest authors of draft guidelines on the management of patients with the condition.
The guidelines, not ready for prime time, have yet to be reviewed or endorsed by the American College of Rheumatology (ACR) and the Spondylitis Association of America, or the SpondyloArthritis Research and Treatment Network (SPARTAN), and are subject to change, emphasized Dr. Michael M. Ward, senior investigator at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
With that caveat in mind, Dr. Ward presented a sneak peek at the guidelines to a standing-room only crowd at the ACR annual meeting in Boston.
Some definitions
The guidelines offer recommendations on the management of patients with active and stable ankylosing spondylitis (AS) and axial spondyloarthropathies (axSpA) that are symptomatic but without radiographic evidence (nonradiographic, or nr-axSpA).
Active AS is defined as disease that causes symptoms at an unacceptably burdensome level as reported by the patient that are judged by the examining clinician to be caused by AS. The same definition also applies to nr-axSpA.
Stable disease is defined as either an asymptomatic state or symptoms that were previously bothersome but are currently at an acceptable level as reported by the patient. The patient had to have had bothersome symptoms for at least 6 months before entering the stable disease state. This definition is also applicable to stable nr-axSpA.
The investigators considered the best available evidence on the use of NSAIDs (running the gamut from aspirin to tolmetin), slow-acting antirheumatic agents such as methotrexate, glucocorticoids (prednisone and others), tumor necrosis factor (TNF) inhibitors, such as adalimumab, etanercept, and others), and non-TNF biologic agents (abatacept, rituximab, tocilizumab, and others).
Active AS
Dr. Ward presented a management flow tree for patients with active AS, starting with a strong recommendation for an NSAID, conditionally recommended to be used continuously. The authors felt, however, that there was not enough evidence to support the use of one NSAID over another. They also strongly recommended physical therapy, with less robust recommendations for active than for passive exercise and for exercises performed in water rather than on land. The latter recommendation is based on the fact that, although water-based exercises have been shown to be as good as or better than dry land exercises for relieving symptoms, water-based exercise may be impractical for many patients, Dr. Ward noted.
For patients whose disease remains active despite NSAIDs and exercise, the committee strongly recommends use of a tumor necrosis factor inhibitor (TNFi) (no specific agent preferred). If a patient on a TNFi has recurrent iritis, the guidelines have a conditional recommendation for the use of infliximab or adalimumab. For patients with inflammatory bowel disease (IBD), the authors conditionally recommend a TNFi monoclonal antibody as opposed to etanercept.
If the disease remains active on a TNFi, an alternative TNFi can be considered.
“For patients who have contraindications to TNF inhibitors, we considered the choice between adding a slow-acting drug such as sulfasalazine or pamidronate or treating with a non-TNF biologic. Of course, there are no head-to-head trials between those two options, so based on the indirect evidence that’s available, the committee voted for a conditional recommendation against the use of a non-TNF biologic in favor of a slow-acting drug in that setting,” Dr. Ward said.
If there are no contraindications to a TNF inhibitor, however, the committee strongly favored the use of a TNF inhibitor over a slow-acting agent, he emphasized.
For patients who have isolated sacroiliitis, peripheral arthritis, or enthesis, the committee provisionally recommends local injection of a glucocorticoid, with cautions to use infrequently and only if two or fewer joints are involved in peripheral arthritis, and avoidance of injection of the Achilles, patellar, or quadriceps tendons in patients with enthesitis.
For all patients, the guidelines half-heartedly recommend monitoring validated axSpA disease activity measures and C-reactive protein and erythrocyte sedimentation rate (ESR). The group also conditionally supported unsupervised back exercises, formal group or individual self-management education, and fall evaluation and counseling.
Committee members strongly felt that systemic glucocorticoids should not be used in patients with active axSpA, except in cases where a short-term course with quick taper may be helpful, such as in patients with peripheral flare, or during pregnancy or a concomitant IBD flare.
Stable AS
“For patients with stable ankylosing spondylitis who are on combination therapy, either combination therapy with NSAIDs and a TNF inhibitor, or a slow-acting drug and a TNF inhibitor, the committee voted against continuation of a combination in favor of TNF monotherapy. It’s a conditional recommendation, so there certainly would be situations where one would not want to do that, but in general the committee thought that was the preferable approach, balancing the benefits and potential risks of combination therapy against monotherapy in patients with stable AS,” Dr. Ward said.
The committee members strongly supported physical therapy in patients with stable AS and gave a conditional nod to monitoring, back exercises, group support, and fall counseling.
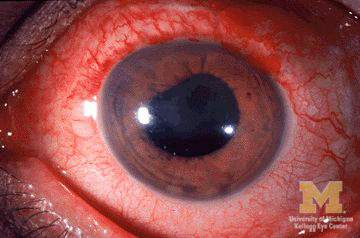
For patients with stable AS and advanced hip arthritis, hip replacement is strongly recommended. Recommendations for and against other special conditions include severe kyphosis (strongly against elective spine osteotomy except in specialized centers), acute iritis (strong support for an ophthalmology consultant), recurrent iritis (conditional support for at home use of a topical glucocorticoid under the supervision of an eye care provider, and use of infliximab or adalimumab over etanercept), and IBD (strong recommendation for TNFi monoclonals over etanercept and conditional endorsement of no preferred NSAID).
Active nr-axSpA
Recommendations for the treatment of nr-axSpA are essentially identical to those for treating active AS, Dr. Ward noted, except that in contrast to active AS, where the recommendation is strongly in favor of TNF inhibitors, the committee gave only a conditional recommendation for the use of a TNF inhibitor in this clinical situation.
Stable nr-axSpA
For patients with stable nr-axSpA, the recommendations are strongly in favor of NSAID use, with a conditional suggestion to use on demand. The recommendations also are conditionally against combination therapy with either an NSAID or slow-acting agent plus a TNF inhibitor, with a conditional approval for TNF inhibitor monotherapy instead. The committee strongly supported physical therapy for these patients and gave a lukewarm embrace of monitoring for disease activity, CRP, or ESR.
Dr. Ward noted that the guidelines are designed to help clinicians with treatment decisions for the typical patient with AS or nr-axSpA, and do not address the needs of all populations or all clinical circumstances or contingencies.
He also noted that for many of the questions the committee members tried to address, high-quality evidence was limited.
Dr. Ward did not mention a projected publication date for the guidelines. He had no relevant financial conflicts to disclose.